Hereditas(Beijing) ›› 2023, Vol. 45 ›› Issue (11): 1074-1084.doi: 10.16288/j.yczz.23-166
• Research Article • Previous Articles
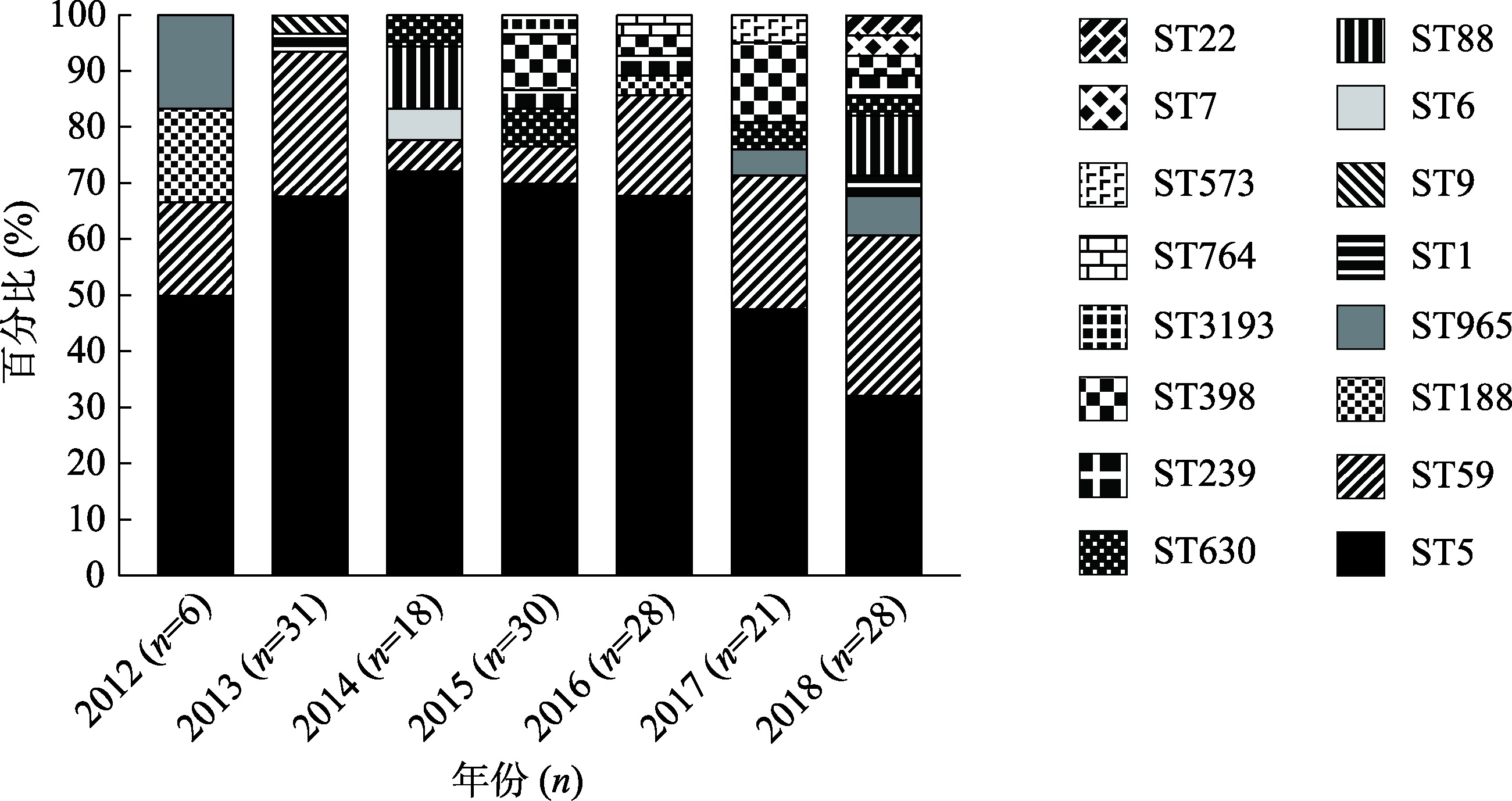
Molecular epidemiology and change trend of methicillin-resistant Staphylococcus aureus from invasive infections of a hospital in Hangzhou from 2012 to 2018
Yunying Zhu( ), Yuan Wang, Tingting Xiao, Jinru Ji, Ping Shen, Yonghong Xiao(
), Yuan Wang, Tingting Xiao, Jinru Ji, Ping Shen, Yonghong Xiao( )
)
- State Key Laboratory for Diagnosis and Treatment of Infectious Diseases, National Clinical Research Center for Infectious Diseases, Collaborative Innovation Center for Diagnosis and Treatment of Infectious Diseases, The First Affiliated Hospital, Zhejiang University School of Medicine,Hangzhou 310003, China
-
Received:2023-06-19Revised:2023-09-09Online:2023-11-20Published:2023-09-20 -
Contact:Yonghong Xiao E-mail:21818043@zju.edu.cn;xiao-yonghong@163.com -
Supported by:National Natural Science Foundation of China(81971984);Key Research and Development program of Zhejiang province(2021C03068);Research Project of Jinan Microecological Biomedicine Shandong Laboratory(JNL-2022006B)
Cite this article
Yunying Zhu, Yuan Wang, Tingting Xiao, Jinru Ji, Ping Shen, Yonghong Xiao. Molecular epidemiology and change trend of methicillin-resistant Staphylococcus aureus from invasive infections of a hospital in Hangzhou from 2012 to 2018[J]. Hereditas(Beijing), 2023, 45(11): 1074-1084.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
Table 1
ST-SCCmec-spa molecular types of 162 MRSA isolates"
| ST分型 | SCCmec | spa | 菌株数(n) | 百分比(%) | ST分型 | SCCmec | spa | 菌株数(n) | 百分比(%) |
|---|---|---|---|---|---|---|---|---|---|
| ST5 | II | t311 | 81 | 50.0 | ST88 | III | t7637 | 1 | 0.6 |
| ST5 | II | t002 | 5 | 3.1 | ST88 | V | t2526 | 1 | 0.6 |
| ST5 | II | t2460 | 3 | 1.9 | ST630 | II | t4549 | 4 | 2.5 |
| ST5 | II | t494 | 1 | 0.6 | ST630 | V | t4549 | 1 | 0.6 |
| ST5 | II | t2731 | 1 | 0.6 | ST965 | NT | t062 | 2 | 1.2 |
| ST5 | II | t3235 | 1 | 0.6 | ST965 | IVa | t062 | 1 | 1.2 |
| ST5 | NT | t311 | 2 | 1.2 | ST965 | II | t062 | 1 | 0.6 |
| ST5 | IVa | t693 | 1 | 0.6 | ST239 | III | t030 | 2 | 1.2 |
| ST5 | V | t319 | 1 | 0.6 | ST239 | NT | t421 | 1 | 0.6 |
| ST59 | IVa | t437 | 18 | 11.1 | ST1 | IVa | t127 | 1 | 0.6 |
| ST59 | IVa | t172 | 4 | 2.5 | ST1 | NT | t127 | 1 | 0.6 |
| ST59 | IVa | t441 | 2 | 1.2 | ST188 | I | t189 | 1 | 0.6 |
| ST59 | IVa | t163 | 1 | 0.6 | ST188 | IVa | t3887 | 1 | 0.6 |
| ST59 | NT | t437 | 3 | 1.8 | ST6 | NT | t701 | 1 | 0.6 |
| ST59 | V | t437 | 1 | 0.6 | ST7 | IVa | t091 | 1 | 0.6 |
| ST59 | V | t4135 | 1 | 0.6 | ST9 | NT | t899 | 1 | 0.6 |
| ST398 | NT | t034 | 7 | 4.3 | ST22 | NT | t309 | 1 | 0.6 |
| ST398 | II | t034 | 1 | 0.6 | ST573 | IVa | t127 | 1 | 0.6 |
| ST88 | NT | t2310 | 1 | 0.6 | ST764 | II | t045 | 1 | 0.6 |
| ST88 | NT | t7637 | 1 | 0.6 | ST3193 | IVa | t172 | 1 | 0.6 |
| ST88 | II | t15047 | 1 | 0.6 |
Table 2
Molecular typing of 28 PVL-positive MRSA isolates"
| PVL阳性的分子分型 | 菌株数(n) | 百分比(%) |
|---|---|---|
| ST59-IVa-t437 | 8 | 28.6 |
| ST5-II-t311 | 4 | 14.3 |
| ST59-NT-t437 | 2 | 7.1 |
| ST5-II-t2460 | 1 | 3.6 |
| ST59-IVa-t172 | 1 | 3.6 |
| ST59-IVa-t441 | 1 | 3.6 |
| ST59-V-437 | 1 | 3.6 |
| ST59-V-t4135 | 1 | 3.6 |
| ST398-II-t034 | 1 | 3.6 |
| ST88-NT-t2310 | 1 | 3.6 |
| ST88-NT-t7637 | 1 | 3.6 |
| ST88-III-t7637 | 1 | 3.6 |
| ST88-V-2526 | 1 | 3.6 |
| ST965-IVa-t062 | 1 | 3.6 |
| ST6-NT-t701 | 1 | 3.6 |
| ST22-NT-t309 | 1 | 3.6 |
| ST3193-IVa-t172 | 1 | 3.6 |
Table 3
Antibiotic resistance of 162 MRSA isolates"
| 抗菌药物 | 耐药株数(%) | 中介株数(%) | 敏感株数(%) |
|---|---|---|---|
| 克林霉素(CLI) | 50(30.9) | 1(0.6) | 111(68.5) |
| 红霉素(ERY) | 138(85.2) | 5(3.1) | 19(11.7) |
| 庆大霉素(GEN) | 9(5.6) | 14(8.6) | 139(85.8) |
| 环丙沙星(CIP) | 107(66.0) | 6(3.7) | 49(30.2) |
| 左氧氟沙星(LVX) | 104(64.2) | 3(1.9) | 55(34.0) |
| 莫西沙星(MXF) | 102(63.0) | 6(3.7) | 54(33.3) |
| 利福平(RIF) | 5(3.1) | 1(0.6) | 156(96.3) |
| 四环素(TCY) | 69(42.6) | - | 93(57.4) |
| 复方新诺明(SXT) | 5(3.1) | - | 157(96.9) |
| 利奈唑胺(LZD) | - | - | 162(100) |
| 替加环素(TGC) | - | - | 162(100) |
| 万古霉素(VAN) | - | - | 162(100) |
Table 4
Antibiotic resistance of MRSA isolates by ST types"
| ST分型 | 菌株数 | 耐药率(%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 克林霉素(CLI) | 红霉素(ERY) | 庆大霉素(GEN) | 环丙沙星(CIP) | 左氧氟沙星(LVX) | 莫西沙星(MFX) | 利福平(RIF) | 四环素(TCY) | 复方新诺明(SXT) | ||
| ST5 | 96 | 20.8 | 100.0 | 16.7 | 99.0 | 99.0 | 99.0 | 3.1 | 54.2 | 0.0 |
| ST59 | 30 | 73.3 | 76.7 | 0.0 | 20.0 | 6.7 | 6.7 | 0.0 | 30.0 | 0.0 |
| ST398 | 8 | 25.0 | 50.0 | 0.0 | 12.5 | 12.5 | 12.5 | 12.5 | 12.5 | 0.0 |
| ST630 | 5 | 0.0 | 40.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| ST965 | 4 | 25.0 | 100.0 | 25.0 | 50.0 | 25.0 | 50.0 | 0.0 | 25.0 | 25.0 |
| ST239 | 3 | 66.7 | 100.0 | 66.7 | 66.7 | 66.7 | 66.7 | 66.7 | 66.7 | 33.3 |
| ST1 | 2 | 0.0 | 100.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| ST188 | 2 | 50.0 | 100.0 | 50.0 | 100.0 | 100.0 | 100.0 | 0.0 | 50.0 | 50.0 |
| ST6 | 1 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| ST7 | 1 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 100.0 | 0.0 |
| ST9 | 1 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 0.0 | 100.0 | 100.0 |
| ST22 | 1 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| ST573 | 1 | 0.0 | 100.0 | 0.0 | 100.0 | 100.0 | 100.0 | 0.0 | 0.0 | 0.0 |
| ST764 | 1 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 0.0 | 100.0 | 0.0 |
| ST3193 | 1 | 100.0 | 100.0 | 0.0 | 100.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Total | 162 | 31.5 | 88.3 | 14.2 | 69.8 | 66.0 | 66.7 | 3.7 | 42.6 | 3.1 |
| [1] |
Mehraj J, Witte W, Akmatov MK, Layer F, Werner G, Krause G. Epidemiology of Staphylococcus aureus nasal carriage patterns in the community. Curr Top Microbiol Immunol, 2016, 398: 55-87.
doi: 10.1007/82_2016_497 pmid: 27370344 |
| [2] |
Hu FP, Guo Y, Zhu DM, Wang F, Jiang XF, Xu YC, Zhang XJ, Zhang ZX, Ji P, Xie Y, Kang M, Wang CQ, Wang AM, Xu YH, Shen JL, Sun ZY, Chen ZJ, Ni YX, Sun JY, Chu YZ, Tian SF, Hu ZD, Li J, Yu YS, Lin J, Shan B, Du Y, Guo SF, Wei LH, Zou FM, Zhang H, Wang C, Hu YJ, Ai XM, Zhuo C, Su DH, Wang RZ, Fang H, Yu BX, Zhao Y, Gong P, Guo DW, Zhao JY, Liu WE, Li YM, Jin Y, Shao CH, Wen KZ, Zhang YR, Xu XS, Yan C, Yu H, Huang XN, Wang SM, Chu YF, Zhang LX, Ma J, Zhou SP, Zhou Y, Zhu L, Meng JH, Dong F, Zheng HY, Shen H, Zhou WQ, Jia W, Li G, Wu JS, Lu YM, Li JH, Liu JS, Liao LF, Gu HQ, Jiang L, He W, Xue SH, Feng J, Dou R, Yue CL. CHINET surveillance of bacterial resistance in China:2018 report. Chin J Infect Chemother, 2020, 20(1): 1-10.
doi: 10.16718/j.1009-7708.2020.01.001 |
|
胡付品, 郭燕, 朱德妹, 汪复, 蒋晓飞, 徐英春, 张小江, 张朝霞, 季萍, 谢轶, 康梅, 王传清, 王爱敏, 徐元宏, 沈继录, 孙自镛, 陈中举, 倪语星, 孙景勇, 褚云卓, 田素飞, 胡志东, 李金, 俞云松, 林洁, 单斌, 杜艳, 郭素芳, 魏莲花, 邹凤梅, 张泓, 王春, 胡云建, 艾效曼, 卓超, 苏丹虹, 汪瑞忠, 房华, 俞碧霞, 赵勇, 龚萍, 郭大文, 赵金英, 刘文恩, 李艳明, 金炎, 邵春红, 温开镇, 张贻荣, 徐雪松, 鄢超, 喻华, 黄湘宁, 王山梅, 楚亚菲, 张利侠, 马娟, 周树平, 周艳, 朱镭, 孟晋华, 董芳, 郑红艳, 沈瀚, 周万青, 贾伟, 李刚, 吴劲松, 卢月梅, 李继红, 刘江山, 廖龙凤, 顾洪芹, 姜琳, 贺雯, 薛顺虹, 冯佼, 窦睿, 岳春雷. 2018年CHINET中国细菌耐药性监测. 中国感染与化疗杂志, 2020, 20(1): 1-10.
doi: 10.16718/j.1009-7708.2020.01.001 |
|
| [3] |
Wang D, Xie KP, Zou D, Meng MZ, Xie MJ. Inhibitory effects of silybin on the efflux pump of methicillin- resistant Staphylococcus aureus. Mol Med Rep, 2018, 18(1): 827-833.
doi: 10.3892/mmr.2018.9021 pmid: 29845191 |
| [4] | Lakhundi S, Zhang KY. Methicillin-resistant Staphylococcus aureus: molecular characterization, evolution, and epidemiology. Clin Microbiol Rev, 2018, 31(4): e00020-18. |
| [5] |
Cassini A, Högberg LD, Plachouras D, Quattrocchi A, Hoxha A, Simonsen GS, Colomb-Cotinat M, Kretzschmar ME, Devleesschauwer B, Cecchini M, Ouakrim DA, Oliveira TC, Struelens MJ, Suetens C, Monnet DL. Burden of AMR Collaborative Group. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: a population-level modelling analysis. Lancet Infect Dis, 2019, 19(1): 56-66.
doi: S1473-3099(18)30605-4 pmid: 30409683 |
| [6] |
Boyce JM, Cookson B, Christiansen K, Hori S, Vuopio-Varkila J, Kocagöz S, Oztop AY, Vandenbroucke- Grauls CMJE, Harbarth S, Pittet D. Meticillin-resistant Staphylococcus aureus. Lancet Infect Dis, 2005, 5(10): 653-663.
doi: 10.1016/S1473-3099(05)70243-7 pmid: 16183520 |
| [7] |
Song JH, Hsueh PR, Chung DR, Ko KS, Kang CI, Peck KR, Yeom JS, Kim SW, Chang HH, Kim YS, Jung SI, Son JS, So TM, Lalitha MK, Yang YH, Huang SG, Wang H, Lu Q, Carlos CC, Perera JA, Chiu CH, Liu JW, Chongthaleong A, Thamlikitkul V, Van PH; ANSORP Study Group. Spread of methicillin-resistant Staphylococcus aureus between the community and the hospitals in Asian countries: an ANSORP study. J Antimicrob Chemother, 2011, 66(5): 1061-1069.
doi: 10.1093/jac/dkr024 |
| [8] |
Hu FP, Guo Y, Zhu DM, Wang F, Jiang XF, Xu YC, Zhang XJ, Zhang CX, Ji P, Xie Y, Kang M, Wang CQ, Wang AM, Xu YH, Shen JL, Sun ZY, Chen ZJ, Ni YX, Sun JY, Chu YZ, Tian SF, Hu ZD, Li J, Yu YS, Lin J, Shan B, Du Y, Han Y, Guo S, Wei LH, Wu L, Zhang H, Kong J, Hu YJ, Ai XM, Zhuo C, Su DH, Yang Q, Jia B, Huang W.Resistance trends among clinical isolates in China reported from CHINET surveillance of bacterial resistance, 2005-2014. Clin Microbiol Infect, 2016, 22(Suppl 1): S9-S14.
doi: 10.1016/j.cmi.2016.01.001 |
| [9] |
Holland TL, Arnold C, Fowler VG Jr. Clinical management of Staphylococcus aureus bacteremia: a review. JAMA, 2014, 312(13): 1330-1341.
doi: 10.1001/jama.2014.9743 pmid: 25268440 |
| [10] | David MZ, Daum RS, Bayer AS, Chambers HF, Fowler VG Jr, Miller LG, Ostrowsky B, Baesa A, Boyle-Vavra S, Eells SJ, Garcia-Houchins S, Gialanella P, Macias-Gil R, Rude TH, Ruffin F, Sieth JJ, Volinski J, Spellberg B. Staphylococcus aureus bacteremia at 5 US academic medical centers, 2008-2011: significant geographic variation in community-onset infections. Clin Infect Dis, 2014, 59(6): 798-807. |
| [11] |
Matouskova I, Janout V. Current knowledge of methicillin- resistant Staphylococcus aureus and community- associated methicillin-resistant Staphylococcus aureus. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub, 2008, 152(2): 191-202.
doi: 10.5507/bp.2008.030 pmid: 19219207 |
| [12] |
Wang X, Liu Q, Zhang H, Li X, Huang WC, Fu QH, Li M.Molecular characteristics of community-associated Staphylococcus aureus isolates from pediatric patients with bloodstream infections between 2012 and 2017 in Shanghai, China. Front Microbiol, 2018, 9: 1211.
doi: 10.3389/fmicb.2018.01211 |
| [13] |
Molton JS, Tambyah PA, Ang BSP, Ling ML, Fisher DA. The global spread of healthcare-associated multidrug- resistant bacteria: a perspective from Asia. Clin Infect Dis, 2013, 56(9): 1310-1318.
doi: 10.1093/cid/cit020 pmid: 23334810 |
| [14] |
Liu YD, Wang H, Du N, Shen E, Chen HB, Niu JQ, Ye HF, Chen MJ. Molecular evidence for spread of two major methicillin-resistant Staphylococcus aureus clones with a unique geographic distribution in Chinese hospitals. Antimicrob Agents Chemother, 2009, 53(2): 512-518.
doi: 10.1128/AAC.00804-08 pmid: 19029328 |
| [15] |
Ko KS, Lee JY, Suh JY, Oh WS, Peck KR, Lee NY, Song JH. Distribution of major genotypes among methicillin- resistant Staphylococcus aureus clones in Asian countries. J Clin Microbiol, 2005, 43(1): 421-426.
doi: 10.1128/JCM.43.1.421-426.2005 |
| [16] | Baines SL, Holt KE, Schultz MB, Seemann T, Howden BO, Jensen SO, van Hal SJ, Coombs GW, Firth N, Powell DR, Stinear TP, Howden BP. Convergent adaptation in the dominant global hospital clone ST239 of methicillin- resistant Staphylococcus aureus. mBio, 2015, 6(2): e00080. |
| [17] |
Dai YX, Liu JL, Guo W, Meng HW, Huang Q, He L, Gao QQ, Lv HY, Liu Y, Wang YN, Wang H, Liu Q, Li M.Decreasing methicillin-resistant Staphylococcus aureus (MRSA) infections is attributable to the disappearance of predominant MRSA ST239 clones, Shanghai, 2008-2017. Emerg Microbes Infect, 2019, 8(1): 471-478.
doi: 10.1080/22221751.2019.1595161 |
| [18] |
Kale P, Dhawan B. The changing face of community- acquired methicillin-resistant Staphylococcus aureus. Indian J Med Microbiol, 2016, 34(3): 275-285.
doi: 10.4103/0255-0857.188313 pmid: 27514947 |
| [19] |
Kallen AJ, Mu Y, Bulens S, Reingold A, Petit S, Gershman K, Ray SM, Harrison LH, Lynfield R, Dumyati G, Townes JM, Schaffner W, Patel PR, Fridkin SK,Active Bacterial Core surveillance (ABCs) MRSA Investigators of the Emerging Infections Program. Health care-associated invasive MRSA infections, 2005-2008. JAMA, 2010, 304(6): 641-648.
doi: 10.1001/jama.2010.1115 pmid: 20699455 |
| [20] |
Aanensen DM, Spratt BG. The multilocus sequence typing network: mlst. net. Nucleic Acids Res, 2005, 33(Web Server issue): W728-W733.
doi: 10.1093/nar/gki415 pmid: 15980573 |
| [21] |
Maiden MC, Bygraves JA, Feil E, Morelli G, Russell JE, Urwin R, Zhang Q, Zhou J, Zurth K, Caugant DA, Feavers IM, Achtman M, Spratt BG. Multilocus sequence typing: a portable approach to the identification of clones within populations of pathogenic microorganisms. Proc Natl Acad Sci USA, 1998, 95(6): 3140-3145.
doi: 10.1073/pnas.95.6.3140 pmid: 9501229 |
| [22] |
Kondo Y, Ito T, Ma XX, Watanabe S, Kreiswirth BN, Etienne J, Hiramatsu K. Combination of multiplex PCRs for staphylococcal cassette chromosome mec type assignment: rapid identification system for mec, ccr, and major differences in junkyard regions. Antimicrob Agents Chemother, 2007, 51(1): 264-274.
doi: 10.1128/AAC.00165-06 pmid: 17043114 |
| [23] |
Koreen L, Ramaswamy SV, Graviss EA, Naidich S, Musser JM, Kreiswirth BN. spa typing method for discriminating among Staphylococcus aureus isolates: implications for use of a single marker to detect genetic micro- and macrovariation. J Clin Microbiol, 2004, 42(2): 792-799.
doi: 10.1128/JCM.42.2.792-799.2004 pmid: 14766855 |
| [24] |
Larsen AR, Stegger M, Sørum M. spa typing directly from a mecA, spa and pvl multiplex PCR assay-a cost-effective improvement for methicillin-resistant Staphylococcus aureus surveillance. Clin Microbiol Infect, 2008, 14(6): 611-614.
doi: 10.1111/j.1469-0691.2008.01995.x |
| [25] |
Enright MC, Robinson DA, Randle G, Feil EJ, Grundmann H, Spratt BG. The evolutionary history of methicillin- resistant Staphylococcus aureus (MRSA). Proc Natl Acad Sci USA, 2002, 99(11): 7687-7692.
doi: 10.1073/pnas.122108599 pmid: 12032344 |
| [26] |
Li M, Du X, Villaruz AE, Diep BA, Wang DC, Song Y, Tian YR, Hu JH, Yu FY, Lu Y, Otto M. MRSA epidemic linked to a quickly spreading colonization and virulence determinant. Nat Med, 2012, 18(5): 816-819.
doi: 10.1038/nm.2692 pmid: 22522561 |
| [27] |
David MZ, Daum RS. Community-associated methicillin- resistant Staphylococcus aureus: epidemiology and clinical consequences of an emerging epidemic. Clin Microbiol Rev, 2010, 23(3): 616-687.
doi: 10.1128/CMR.00081-09 |
| [28] |
Xiao M, Wang H, Zhao Y, Mao LL, Brown M, Yu YS, O'Sullivan MVN, Kong FR, Xu YC. National surveillance of methicillin-resistant Staphylococcus aureus in China highlights a still-evolving epidemiology with 15 novel emerging multilocus sequence types. J Clin Microbiol, 2013, 51(11): 3638-3644.
doi: 10.1128/JCM.01375-13 pmid: 23985906 |
| [29] | Aires de Sousa M, de Lencastre H, Santos Sanches I, Kikuchi K, Totsuka K, Tomasz A. Similarity of antibiotic resistance patterns and molecular typing properties of methicillin-resistant Staphylococcus aureus isolates widely spread in hospitals in New York City and in a hospital in Tokyo, Japan. Microb Drug Resist, 2000, 6(3): 253-258. |
| [30] |
Chung M, Dickinson G, De Lencastre H, Tomasz A. International clones of methicillin-resistant Staphylococcus aureus in two hospitals in Miami, Florida. J Clin Microbiol, 2004, 42(2): 542-547.
doi: 10.1128/JCM.42.2.542-547.2004 pmid: 14766814 |
| [31] |
Wu DD, Wang ZG, Wang HP, Sun L, Chen Y, Ji SJ, Shi KR, Yu YS. Predominance of ST5-II-t311 clone among healthcare-associated methicillin-resistant Staphylococcus aureus isolates recovered from Zhejiang, China. Int J Infect Dis, 2018, 71: 107-112.
doi: S1201-9712(18)30882-8 pmid: 29698703 |
| [32] |
Chen CJ, Huang YC, Su LH, Wu TL, Huang SH, Chien CC, Chen PY, Lu MC, Ko WC.Molecular epidemiology and antimicrobial resistance of methicillin-resistant Staphylococcus aureus bloodstream isolates in Taiwan, 2010. PLoS One, 2014, 9(6): e101184.
doi: 10.1371/journal.pone.0101184 |
| [33] |
Kong HS, Yu F, Zhang WL, Li XF, Wang HX. Molecular epidemiology and antibiotic resistance profiles of methicillin-resistant Staphylococcus aureus strains in a tertiary hospital in China. Front Microbiol, 2017, 8: 838.
doi: 10.3389/fmicb.2017.00838 |
| [34] |
Li XH, Fang F, Zhao J, Lou N, Li CL, Huang T, Li YR. Molecular characteristics and virulence gene profiles of Staphylococcus aureus causing bloodstream infection. Braz J Infect Dis, 2018, 22(6): 487-494.
doi: S1413-8670(18)30970-X pmid: 30594541 |
| [35] |
Chen X, Sun KD, Luo QQ, Duan YT, Chen FX. Emergence and spread of pvl-positive genotypic CA-MRSA ST59 with increased adhesion capacity from wounds in hospitals. J Infect, 2019, 79(6): 612-625.
doi: S0163-4453(19)30299-3 pmid: 31629018 |
| [36] |
Li SG, Sun SJ, Yang CT, Chen HB, Yin YY, Li HN, Zhao CJ, Wang H. The changing pattern of population structure of Staphylococcus aureus from bacteremia in China from 2013 to 2016: ST239-030-MRSA replaced by ST59-t437. Front Microbiol, 2018, 9: 332.
doi: 10.3389/fmicb.2018.00332 |
| [37] |
Molla B, Byrne M, Abley M, Mathews J, Jackson CR, Fedorka-Cray P, Sreevatsan S, Wang P, Gebreyes WA. Epidemiology and genotypic characteristics of methicillin- resistant Staphylococcus aureus strains of porcine origin. J Clin Microbiol, 2012, 50(11): 3687-3693.
doi: 10.1128/JCM.01971-12 |
| [38] |
Khanna T, Friendship R, Dewey C, Weese JS. Methicillin resistant Staphylococcus aureus colonization in pigs and pig farmers. Vet Microbiol, 2008, 128(3-4): 298-303.
doi: 10.1016/j.vetmic.2007.10.006 pmid: 18023542 |
| [39] |
Verhegghe M, Pletinckx LJ, Crombé F, Vandersmissen T, Haesebrouck F, Butaye P, Heyndrickx M, Rasschaert G. Methicillin-resistant Staphylococcus aureus (MRSA) ST398 in pig farms and multispecies farms. Zoonoses Public Health, 2013, 60(5): 366-374.
doi: 10.1111/zph.2013.60.issue-5 |
| [40] |
Ma XX, Ito T, Tiensasitorn C, Jamklang M, Chongtrakool P, Boyle-Vavra S, Daum RS, Hiramatsu K. Novel type of staphylococcal cassette chromosome mec identified in community-acquired methicillin-resistant Staphylococcus aureus strains. Antimicrob Agents Chemother, 2002, 46(4): 1147-1152.
doi: 10.1128/AAC.46.4.1147-1152.2002 pmid: 11897611 |
| No related articles found! |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||