Hereditas(Beijing) ›› 2022, Vol. 44 ›› Issue (4): 289-299.doi: 10.16288/j.yczz.22-030
• Review • Previous Articles Next Articles
Research progress on the role and regulatory mechanism of pathogenic Th17 cells in neuroinflammation
Hongyu Dai1,2( ), Dong Ji1,2, Cheng Tan1,2, Jie Sun3(
), Dong Ji1,2, Cheng Tan1,2, Jie Sun3( ), Hao Yao1,2(
), Hao Yao1,2( )
)
- 1. Department of Cardiovascular Surgery Center, The Second Affiliated Hospital of Nanjing Medical University, Nanjing 210003, China
2. Department of Anesthesiology, The Second Affiliated Hospital of Nanjing Medical University, Nanjing 210011, China
3. Department of Anesthesiology, Zhongda Hospital, Medical School, Southeast University, Nanjing 210009, China
-
Received:2022-02-12Revised:2022-03-18Online:2022-04-20Published:2022-03-25 -
Contact:Sun Jie,Yao Hao E-mail:daihongyu@njmu.edu.cn;dgsunjie@hotmail.com;yaohao@njmu.edu.cn -
Supported by:Supported by the Provincial Key R&D Program (Social Development) of Science and Technology Department of Jiangsu Province No(SBE2021741263);the 789 Talents Training Program of the Second Affiliated Hospital of Nanjing Medical University No(789ZYRC080236)
Cite this article
Hongyu Dai, Dong Ji, Cheng Tan, Jie Sun, Hao Yao. Research progress on the role and regulatory mechanism of pathogenic Th17 cells in neuroinflammation[J]. Hereditas(Beijing), 2022, 44(4): 289-299.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
| [1] |
Solleiro-Villavicencio H, Rivas-Arancibia S. Effect of chronic oxidative stress on neuroinflammatory response mediated by CD4 +T cells in neurodegenerative diseases. Front Cell Neurosci, 2018, 12:114.
doi: 10.3389/fncel.2018.00114 pmid: 29755324 |
| [2] |
Singh RP, Hasan S, Sharma S, Nagra S, Yamaguchi DT, Wong DTW, Hahn BH, Hossain A. Th17 cells in inflammation and autoimmunity. Autoimmun Rev, 2014, 13(12):1174-1181.
doi: 10.1016/j.autrev.2014.08.019 |
| [3] |
Moser T, Akgün K, Proschmann U, Sellner J, Ziemssen T. The role of TH17 cells in multiple sclerosis: therapeutic implications. Autoimmun Rev, 2020, 19(10):102647.
doi: 10.1016/j.autrev.2020.102647 |
| [4] |
MacMahon Copas AN, McComish SF, Fletcher JM, Caldwell MA. The pathogenesis of Parkinson’s disease: a complex interplay between astrocytes, microglia, and T lymphocytes? Front Neurol, 2021, 12:666737.
doi: 10.3389/fneur.2021.666737 |
| [5] |
Harrington LE, Hatton RD, Mangan PR, Turner H, Murphy TL, Murphy KM, Weaver CT. Interleukin 17-producing CD4+ effector T cells develop via a lineage distinct from the T helper type 1 and 2 lineages. Nat Immunol, 2005, 6(11):1123-1132.
doi: 10.1038/ni1254 pmid: 16200070 |
| [6] |
Omenetti S, Bussi C, Metidji A, Iseppon A, Lee S, Tolaini M, Li Y, Kelly G, Chakravarty P, Shoaie S, Gutierrez MG, Stockinger B. The intestine harbors functionally distinct homeostatic tissue-resident and inflammatory Th17 cells. Immunity, 2019, 51(1): 77-89.e6.
doi: S1074-7613(19)30224-9 pmid: 31229354 |
| [7] |
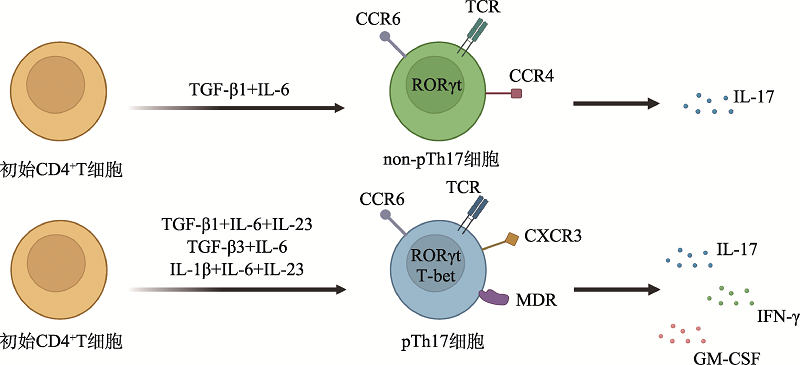
Lee Y, Awasthi A, Yosef N, Quintana FJ, Xiao S, Peters A, Wu C, Kleinewietfeld M, Kunder S, Hafler DA, Sobel RA, Regev A, Kuchroo VK. Induction and molecular signature of pathogenic TH17 cells. Nat Immunol, 2012, 13(10):991-999.
doi: 10.1038/ni.2416 |
| [8] |
Ghoreschi K, Laurence A, Yang XP, Hirahara K, O’Shea JJ. T helper 17 cell heterogeneity and pathogenicity in autoimmune disease. Trends Immunol, 2011, 32(9):395-401.
doi: 10.1016/j.it.2011.06.007 pmid: 21782512 |
| [9] |
Stockinger B, Omenetti S. The dichotomous nature of T helper 17 cells. Nat Rev Immunol, 2017, 17(9):535-544.
doi: 10.1038/nri.2017.50 pmid: 28555673 |
| [10] |
Dankers W, Davelaar N, van Hamburg JP, van de Peppel J, Colin EM, Lubberts E. Human memory Th17 cell populations change into anti-inflammatory cells with regulatory capacity upon exposure to active vitamin D. Front Immunol, 2019, 10:1504.
doi: 10.3389/fimmu.2019.01504 pmid: 31379807 |
| [11] |
O'Connor W, Kamanaka M, Booth CJ, Town T, Nakae S, Iwakura Y, Kolls JK, Flavell RA. A protective function for interleukin 17A in T cell-mediated intestinal inflammation. Nat Immunol, 2009, 10(6):603-609.
doi: 10.1038/ni.1736 pmid: 19448631 |
| [12] |
Wang C, Yosef N, Gaublomme J, Wu C, Lee Y, Clish CB, Kaminski J, Xiao S, Meyer Zu Horste G, Pawlak M, Kishi Y, Joller N, Karwacz K, Zhu C, Ordovas-Montanes M, Madi A, Wortman I, Miyazaki T, Sobel RA, Park H, Regev A, Kuchroo VK. CD5L/AIM regulates lipid biosynthesis and restrains Th17 cell pathogenicity. Cell, 2015, 163(6):1413-1427.
doi: 10.1016/j.cell.2015.10.068 |
| [13] |
Aschenbrenner D, Foglierini M, Jarrossay D, Hu D, Weiner HL, Kuchroo VK, Lanzavecchia A, Notarbartolo S, Sallusto F. An immunoregulatory and tissue-residency program modulated by c-MAF in human TH17 cells. Nat Immunol, 2018, 19(10):1126-1136.
doi: 10.1038/s41590-018-0200-5 pmid: 30201991 |
| [14] |
McGeachy MJ, Bak-Jensen KS, Chen Y, Tato CM, Blumenschein W, McClanahan T, Cua DJ. TGF-β and IL-6 drive the production of IL-17 and IL-10 by T cells and restrain T(H)-17 cell-mediated pathology. Nat Immunol, 2007, 8(12):1390-1397.
doi: 10.1038/ni1539 pmid: 17994024 |
| [15] |
Codarri L, Gyülvészi G, Tosevski V, Hesske L, Fontana A, Magnenat L, Suter T, Becher B. RORγt drives production of the cytokine GM-CSF in helper T cells, which is essential for the effector phase of autoimmune neuroinflammation. Nat Immunol, 2011, 12(6):560-567.
doi: 10.1038/ni.2027 pmid: 21516112 |
| [16] |
Sonderegger I, Iezzi G, Maier R, Schmitz N, Kurrer M, Kopf M. GM-CSF mediates autoimmunity by enhancing IL-6-dependent Th17 cell development and survival. J Exp Med, 2008, 205(10):2281-2294.
doi: 10.1084/jem.20071119 |
| [17] |
Duhen R, Glatigny S, Arbelaez CA, Blair TC, Oukka M, Bettelli E. Cutting edge: the pathogenicity of IFN-γ- producing Th17 cells is independent of T-bet. J Immunol, 2013, 190(9):4478-4482.
doi: 10.4049/jimmunol.1203172 |
| [18] |
van Langelaar J, van der Vuurst de Vries RM, Janssen M, Wierenga-Wolf AF, Spilt IM, Siepman TA, Dankers W, Verjans GMGM, de Vries HE, Lubberts E, Hintzen RQ, van Luijn MM. T helper 17.1 cells associate with multiple sclerosis disease activity: perspectives for early intervention. Brain, 2018, 141(5):1334-1349.
doi: 10.1093/brain/awy069 pmid: 29659729 |
| [19] |
Paulissen SMJ, van Hamburg JP, Dankers W, Lubberts E. The role and modulation of CCR6 + Th17 cell populations in rheumatoid arthritis. Cytokine, 2015, 74(1):43-53.
doi: 10.1016/j.cyto.2015.02.002 pmid: 25828206 |
| [20] |
Basdeo SA, Cluxton D, Sulaimani J, Moran B, Canavan M, Orr C, Veale DJ, Fearon U, Fletcher JM. Ex-Th17 (nonclassical th1) cells are functionally distinct from classical Th1 and Th17 cells and are not constrained by regulatory T cells. J Immunol, 2017, 198(6):2249-2259.
doi: 10.4049/jimmunol.1600737 |
| [21] |
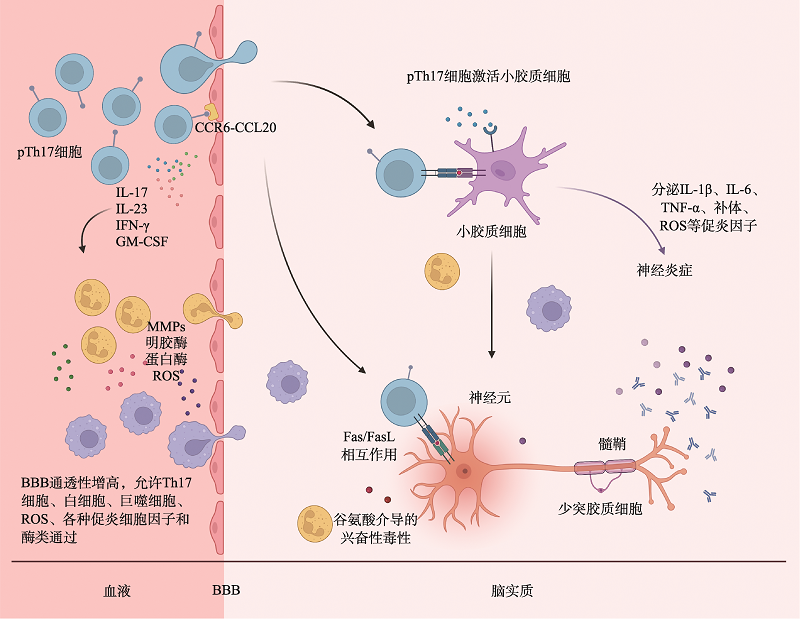
Tahmasebinia F, Pourgholaminejad A. The role of Th17 cells in auto-inflammatory neurological disorders. Prog Neuropsychopharmacol Biol Psychiatry, 2017, 79(Pt B):408-416.
doi: 10.1016/j.pnpbp.2017.07.023 |
| [22] |
Mastorakos P, McGavern D. The anatomy and immunology of vasculature in the central nervous system. Sci Immunol, 2019, 4(37): eaav0492.
doi: 10.1126/sciimmunol.aav0492 |
| [23] |
Profaci CP, Munji RN, Pulido RS, Daneman R. The blood- brain barrier in health and disease: important unanswered questions. J Exp Med, 2020, 217(4):e20190062.
doi: 10.1084/jem.20190062 |
| [24] |
Baumjohann D, Ansel KM. MicroRNA-mediated regulation of T helper cell differentiation and plasticity. Nat Rev Immunol, 2013, 13(9):666-678.
doi: 10.1038/nri3494 pmid: 23907446 |
| [25] |
Breuer J, Korpos E, Hannocks MJ, Schneider-Hohendorf T, Song J, Zondler L, Herich S, Flanagan K, Korn T, Zarbock A, Kuhlmann T, Sorokin L, Wiendl H, Schwab N. Blockade of MCAM/CD146 impedes CNS infiltration of T cells over the choroid plexus. J Neuroinflammation, 2018, 15(1):236.
doi: 10.1186/s12974-018-1276-4 |
| [26] |
Cipollini V, Anrather J, Orzi F, Iadecola C. Th17 and cognitive impairment: possible mechanisms of action. Front Neuroanat, 2019, 13:95.
doi: 10.3389/fnana.2019.00095 pmid: 31803028 |
| [27] | Haqqani AS, Stanimirovic DB. Intercellular interactomics of human brain endothelial cells and th17 lymphocytes: a novel strategy for identifying therapeutic targets of CNS inflammation. Cardiovasc Psychiatry Neurol, 2011, 2011:175364. |
| [28] |
Witowski J, Pawlaczyk K, Breborowicz A, Scheuren A, Kuzlan-Pawlaczyk M, Wisniewska J, Polubinska A, Friess H, Gahl GM, Frei U, Jörres A. IL-17 stimulates intraperitoneal neutrophil infiltration through the release of GRO alpha chemokine from mesothelial cells. J Immunol, 2000, 165(10):5814-5821.
pmid: 11067941 |
| [29] |
Huppert J, Closhen D, Croxford A, White R, Kulig P, Pietrowski E, Bechmann I, Becher B, Luhmann HJ, Waisman A, Kuhlmann CRW. Cellular mechanisms of IL-17-induced blood-brain barrier disruption. FASEB J, 2010, 24(4):1023-1034.
doi: 10.1096/fj.09-141978 pmid: 19940258 |
| [30] |
Kawanokuchi J, Shimizu K, Nitta A, Yamada K, Mizuno T, Takeuchi H, Suzumura A. Production and functions of IL-17 in microglia. J Neuroimmunol, 2008, 194(1-2):54-61.
doi: 10.1016/j.jneuroim.2007.11.006 pmid: 18164424 |
| [31] |
Debnath M, Berk M. Th17 pathway-mediated immunopathogenesis of schizophrenia: mechanisms and implications. Schizophr Bull, 2014, 40(6):1412-1421.
doi: 10.1093/schbul/sbu049 |
| [32] |
Michinaga S, Koyama Y. Dual roles of astrocyte-derived factors in regulation of blood-brain barrier function after brain damage. Int J Mol Sci, 2019, 20(3):571.
doi: 10.3390/ijms20030571 |
| [33] |
Meares GP, Ma XY, Qin HW, Benveniste EN. Regulation of CCL20 expression in astrocytes by IL-6 and IL-17. Glia, 2012, 60(5):771-781.
doi: 10.1002/glia.22307 |
| [34] |
Das Sarma J, Ciric B, Marek R, Sadhukhan S, Caruso ML, Shafagh J, Fitzgerald DC, Shindler KS, Rostami A. Functional interleukin-17 receptor A is expressed in central nervous system glia and upregulated in experimental autoimmune encephalomyelitis. J Neuroinflammation, 2009, 6:14.
doi: 10.1186/1742-2094-6-14 |
| [35] |
Kang ZZ, Altuntas CZ, Gulen MF, Liu CN, Giltiay N, Qin HW, Liu LP, Qian W, Ransohoff RM, Bergmann C, Stohlman S, Tuohy VK, Li XX. Astrocyte-restricted ablation of interleukin-17-induced Act1-mediated signaling ameliorates autoimmune encephalomyelitis. Immunity, 2010, 32(3):414-425.
doi: 10.1016/j.immuni.2010.03.004 |
| [36] |
Williams JL, Manivasagam S, Smith BC, Sim J, Vollmer LL, Daniels BP, Russell JH, Klein RS. Astrocyte-T cell crosstalk regulates region-specific neuroinflammation. Glia, 2020, 68(7):1361-1374.
doi: 10.1002/glia.23783 pmid: 31961459 |
| [37] |
Tzartos JS, Craner MJ, Friese MA, Jakobsen KB, Newcombe J, Esiri MM, Fugger L. IL-21 and IL-21 receptor expression in lymphocytes and neurons in multiple sclerosis brain. Am J Pathol, 2011, 178(2):794-802.
doi: 10.1016/j.ajpath.2010.10.043 pmid: 21281812 |
| [38] |
Birkner K, Wasser B, Ruck T, Thalman C, Luchtman D, Pape K, Schmaul S, Bitar L, Krämer-Albers EM, Stroh A, Meuth SG, Zipp F, Bittner S. β1-Integrin- and KV1.3 channel-dependent signaling stimulates glutamate release from Th17 cells. J Clin Invest, 2020, 130(2):715-732.
doi: 10.1172/JCI126381 |
| [39] |
Williams PR, Marincu BN, Sorbara CD, Mahler CF, Schumacher AM, Griesbeck O, Kerschensteiner M, Misgeld T. A recoverable state of axon injury persists for hours after spinal cord contusion in vivo. Nat Commun, 2014, 5:5683.
doi: 10.1038/ncomms6683 pmid: 25511170 |
| [40] | Wu B, Wan YS. Molecular control of pathogenic Th17 cells in autoimmune diseases. Int Immunopharmacol, 2020, 80:106187. |
| [41] |
Hirota K, Duarte JH, Veldhoen M, Hornsby E, Li Y, Cua DJ, Ahlfors H, Wilhelm C, Tolaini M, Menzel U, Garefalaki A, Potocnik AJ, Stockinger B. Fate mapping of IL-17-producing T cells in inflammatory responses. Nat Immunol, 2011, 12(3):255-263.
doi: 10.1038/ni.1993 pmid: 21278737 |
| [42] |
Jain R, Chen Y, Kanno Y, Joyce-Shaikh B, Vahedi G, Hirahara K, Blumenschein WM, Sukumar S, Haines CJ, Sadekova S, McClanahan TK, McGeachy MJ, O'Shea JJ, Cua DJ. Interleukin-23-induced transcription factor Blimp-1 promotes pathogenicity of T helper 17 cells. Immunity, 2016, 44(1):131-142.
doi: 10.1016/j.immuni.2015.11.009 |
| [43] |
Wu C, Yosef N, Thalhamer T, Zhu C, Xiao S, Kishi Y, Regev A, Kuchroo VK. Induction of pathogenic TH17 cells by inducible salt-sensing kinase SGK1. Nature, 2013, 496(7446):513-517.
doi: 10.1038/nature11984 |
| [44] |
Haase S, Wilck N, Kleinewietfeld M, Müller DN, Linker RA. Sodium chloride triggers Th17 mediated autoimmunity. J Neuroimmunol, 2019, 329:9-13.
doi: 10.1016/j.jneuroim.2018.06.016 |
| [45] |
Fleetwood AJ, Cook AD, Hamilton JA. Functions of granulocyte-macrophage colony-stimulating factor. Crit Rev Immunol, 2005, 25(5):405-428.
pmid: 16167889 |
| [46] |
El-Behi M, Ciric B, Dai H, Yan YP, Cullimore M, Safavi F, Zhang GX, Dittel BN, Rostami A. The encephalitogenicity of T(H)17 cells is dependent on IL-1- and IL-23-induced production of the cytokine GM-CSF. Nat Immunol, 2011, 12(6):568-575.
doi: 10.1038/ni.2031 |
| [47] |
Fujio K, Komai T, Inoue M, Morita K, Okamura T, Yamamoto K. Revisiting the regulatory roles of the TGF-β family of cytokines. Autoimmun Rev, 2016, 15(9):917-922.
doi: 10.1016/j.autrev.2016.07.007 |
| [48] |
Bettelli E, Carrier Y, Gao WD, Korn T, Strom TB, Oukka M, Weiner HL, Kuchroo VK. Reciprocal developmental pathways for the generation of pathogenic effector TH17 and regulatory T cells. Nature, 2006, 441(7090):235-238.
doi: 10.1038/nature04753 |
| [49] |
Gutcher I, Donkor MK, Ma Q, Rudensky AY, Flavell RA, Li MO. Autocrine transforming growth factor-β1 promotes in vivo Th17 cell differentiation. Immunity, 2011, 34(3):396-408.
doi: 10.1016/j.immuni.2011.03.005 pmid: 21435587 |
| [50] |
Mangan PR, Harrington LE, O'Quinn DB, Helms WS, Bullard DC, Elson CO, Hatton RD, Wahl SM, Schoeb TR, Weaver CT. Transforming growth factor-beta induces development of the T(H)17 lineage. Nature, 2006, 441(7090):231-234.
doi: 10.1038/nature04754 |
| [51] |
Li MO, Wan YY, Flavell RA. T cell-produced transforming growth factor-beta1 controls T cell tolerance and regulates Th1- and Th17-cell differentiation. Immunity, 2007, 26(5):579-591.
doi: 10.1016/j.immuni.2007.03.014 |
| [52] |
Ghoreschi K, Laurence A, Yang XP, Tato CM, McGeachy MJ, Konkel JE, Ramos HL, Wei L, Davidson TS, Bouladoux N, Grainger JR, Chen Q, Kanno Y, Watford WT, Sun HW, Eberl G, Shevach EM, Belkaid Y, Cua DJ, Chen WJ, O'Shea JJ. Generation of pathogenic T(H)17 cells in the absence of TGF-β signalling. Nature, 2010, 467(7318):967-971.
doi: 10.1038/nature09447 |
| [53] |
Chikuma S, Suita N, Okazaki IM, Shibayama S, Honjo T. TRIM28 prevents autoinflammatory T cell development in vivo. Nat Immunol, 2012, 13(6):596-603.
doi: 10.1038/ni.2293 |
| [54] | Wang HX, Zhu DH. Functions of smad and its binding proteins in TGF β signal pathway. Hereditas(Beijing), 2003, 25(4):479-483. |
| 王海霞, 朱大海. Smad及其结合蛋白在TGF β信号传导中的功能. 遗传, 2003, 25(4):479-483. | |
| [55] |
Morianos I, Papadopoulou G, Semitekolou M, Xanthou G. Activin-A in the regulation of immunity in health and disease. J Autoimmun, 2019, 104:102314.
doi: 10.1016/j.jaut.2019.102314 |
| [56] |
Zhang S, Takaku M, Zou LY, Gu AD, Chou WC, Zhang G, Wu B, Kong Q, Thomas SY, Serody JS, Chen X, Xu XJ, Wade PA, Cook DN, Ting JPY, Wan YY. Reversing SKI-SMAD4-mediated suppression is essential for TH17 cell differentiation. Nature, 2017, 551(7678):105-109.
doi: 10.1038/nature24283 |
| [57] |
Wu B, Zhang S, Guo ZL, Bi YM, Zhou MX, Li P, Seyedsadr M, Xu XJ, Li JL, Markovic-Plese S, Wan YY. The TGF-β superfamily cytokine activin-A is induced during autoimmune neuroinflammation and drives pathogenic Th17 cell differentiation. Immunity, 2021, 54(2): 308-323.e6.
doi: 10.1016/j.immuni.2020.12.010 |
| [58] |
Liu HP, Yao SX, Dann SM, Qin HW, Elson CO, Cong YZ. ERK differentially regulates Th17- and Treg-cell development and contributes to the pathogenesis of colitis. Eur J Immunol, 2013, 43(7):1716-1726.
doi: 10.1002/eji.201242889 |
| [59] |
Brereton CF, Sutton CE, Lalor SJ, Lavelle EC, Mills KHG. Inhibition of ERK MAPK suppresses IL-23- and IL-1- driven IL-17 production and attenuates autoimmune disease. J Immunol, 2009, 183(3):1715-1723.
doi: 10.4049/jimmunol.0803851 pmid: 19570828 |
| [60] |
Xu Q, Jin XX, Zheng MZ, Rohila D, Fu GT, Wen ZY, Lou J, Wu SQ, Sloan R, Wang L, Hu H, Gao X, Lu LR. Phosphatase PP2A is essential for TH17 differentiation. Proc Natl Acad Sci USA, 2019, 116(3):982-987.
doi: 10.1073/pnas.1807484116 |
| [61] |
Kozomara A, Birgaoanu M, Griffiths-Jones S. miRBase: from microRNA sequences to function. Nucleic Acids Res, 2019, 47(D1):D155-D162.
doi: 10.1093/nar/gky1141 |
| [62] |
Baumjohann D, Ansel KM. MicroRNA-mediated regulation of T helper cell differentiation and plasticity. Nat Rev Immunol, 2013, 13(9):666-678.
doi: 10.1038/nri3494 pmid: 23907446 |
| [63] |
Chen C, Zhou YF, Wang JQ, Yan YP, Peng LS, Qiu W. Dysregulated microRNA involvement in multiple sclerosis by induction of T helper 17 cell differentiation. Front Immunol, 2018, 9:1256.
doi: 10.3389/fimmu.2018.01256 pmid: 29915595 |
| [64] |
Ichiyama K, Gonzalez-Martin A, Kim BS, Jin HY, Jin W, Xu W, Sabouri-Ghomi M, Xu SB, Zheng P, Xiao CC, Dong C. The microRNA-183-96-182 cluster promotes T helper 17 cell pathogenicity by negatively regulating transcription factor Foxo1 expression. Immunity, 2016, 44(6):1284-1298.
doi: 10.1016/j.immuni.2016.05.015 pmid: 27332731 |
| [65] |
Bamodu OA, Huang WC, Lee WH, Wu A, Wang LS, Hsiao M, Yeh CT, Chao TY. Aberrant KDM5B expression promotes aggressive breast cancer through MALAT1 overexpression and downregulation of hsa-miR-448. BMC Cancer, 2016, 16:160.
doi: 10.1186/s12885-016-2108-5 |
| [66] |
Hong XH, Xu Y, Qiu XF, Zhu YK, Feng X, Ding ZJ, Zhang SF, Zhong LF, Zhuang YF, Su C, Hong XY, Cai JC. MiR-448 promotes glycolytic metabolism of gastric cancer by downregulating KDM2B. Oncotarget, 2016, 7(16):22092-22102.
doi: 10.18632/oncotarget.8020 |
| [67] |
Lou Q, Liu RX, Yang XL, Li WQ, Huang LL, Wei LL, Tan HL, Xiang NL, Chan K, Chen JX, Liu HL. MiR-448 targets IDO1 and regulates CD8 + T cell response in human colon cancer. J Immunother Cancer, 2019, 7(1):210.
doi: 10.1186/s40425-019-0691-0 |
| [68] |
Sasahira T, Kurihara M, Nishiguchi Y, Fujiwara R, Kirita T, Kuniyasu H. NEDD 4 binding protein 2-like 1 promotes cancer cell invasion in oral squamous cell carcinoma. Virchows Arch, 2016, 469(2):163-172.
doi: 10.1007/s00428-016-1955-4 |
| [69] |
Wu RH, He QY, Chen HT, Xu M, Zhao N, Xiao Y, Tu QQ, Zhang WJ, Bi XY. MicroRNA-448 promotes multiple sclerosis development through induction of Th17 response through targeting protein tyrosine phosphatase non-receptor type 2 (PTPN2). Biochem Biophys Res Commun, 2017, 486(3):759-766.
doi: 10.1016/j.bbrc.2017.03.115 |
| [70] |
Keller A, Leidinger P, Lange J, Borries A, Schroers H, Scheffler M, Lenhof HP, Ruprecht K, Meese E. Multiple sclerosis: microRNA expression profiles accurately differentiate patients with relapsing-remitting disease from healthy controls. PLoS One, 2009, 4(10):e7440.
doi: 10.1371/journal.pone.0007440 |
| [71] |
Zhu ED, Wang X, Zheng B, Wang Q, Hao JL, Chen SM, Zhao Q, Zhao LQ, Wu ZZ, Yin ZN. MiR-20b suppresses Th17 differentiation and the pathogenesis of experimental autoimmune encephalomyelitis by targeting RORγt and STAT3. J Immunol, 2014, 192(12):5599-5609.
doi: 10.4049/jimmunol.1303488 |
| [72] |
Chen J, Martindale JL, Abdelmohsen K, Kumar G, Fortina PM, Gorospe M, Rostami A, Yu SG. RNA-binding protein HuR promotes Th17 cell differentiation and can be targeted to reduce autoimmune neuroinflammation. J Immunol, 2020, 204(8):2076-2087.
doi: 10.4049/jimmunol.1900769 |
| [73] |
Chen J, Martindale JL, Cramer C, Gorospe M, Atasoy U, Drew PD, Yu SG. The RNA-binding protein HuR contributes to neuroinflammation by promoting C-C chemokine receptor 6 (CCR6) expression on Th17 cells. J Biol Chem, 2017, 292(35):14532-14543.
doi: 10.1074/jbc.M117.782771 |
| [74] |
Roy DG, Chen J, Mamane V, Ma EH, Muhire BM, Sheldon RD, Shorstova T, Koning R, Johnson RM, Esaulova E, Williams KS, Hayes S, Steadman M, Samborska B, Swain A, Daigneault A, Chubukov V, Roddy TP, Foulkes W, Pospisilik JA, Bourgeois-Daigneault MC, Artyomov MN, Witcher M, Krawczyk CM, Larochelle C, Jones RG. Methionine metabolism shapes T helper cell responses through regulation of epigenetic reprogramming. Cell Metab, 2020, 31(2): 250-266.e9.
doi: 10.1016/j.cmet.2020.01.006 |
| [75] |
Cho JJ, Xu ZW, Parthasarathy U, Drashansky TT, Helm EY, Zuniga AN, Lorentsen KJ, Mansouri S, Cho JY, Edelmann MJ, Duong DM, Gehring T, Seeholzer T, Krappmann D, Uddin MN, Califano D, Wang RL, Jin L, Li HM, Lv DW, Zhou DH, Zhou L, Avram D. Hectd3 promotes pathogenic Th17 lineage through Stat3 activation and Malt1 signaling in neuroinflammation. Nat Commun, 2019, 10(1):701.
doi: 10.1038/s41467-019-08605-3 |
| [76] |
Perfetto SP, Chattopadhyay PK, Roederer M. Seventeen- colour flow cytometry: unravelling the immune system. Nat Rev Immunol, 2004, 4(8):648-655.
doi: 10.1038/nri1416 pmid: 15286731 |
| [77] |
Shalek AK, Satija R, Adiconis X, Gertner RS, Gaublomme JT, Raychowdhury R, Schwartz S, Yosef N, Malboeuf C, Lu D, Trombetta JJ, Gennert D, Gnirke A, Goren A, Hacohen N, Levin JZ, Park H, Regev A. Single-cell transcriptomics reveals bimodality in expression and splicing in immune cells. Nature, 2013, 498(7453):236-240.
doi: 10.1038/nature12172 |
| [78] |
Gaublomme JT, Yosef N, Lee Y, Gertner RS, Yang LV, Wu C, Pandolfi PP, Mak T, Satija R, Shalek AK, Kuchroo VK, Park H, Regev A. Single-cell genomics unveils critical regulators of Th17 cell pathogenicity. Cell, 2015, 163(6):1400-1412.
doi: 10.1016/j.cell.2015.11.009 pmid: 26607794 |
| No related articles found! |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||