Hereditas(Beijing) ›› 2025, Vol. 47 ›› Issue (6): 650-659.doi: 10.16288/j.yczz.24-209
• Review • Previous Articles Next Articles
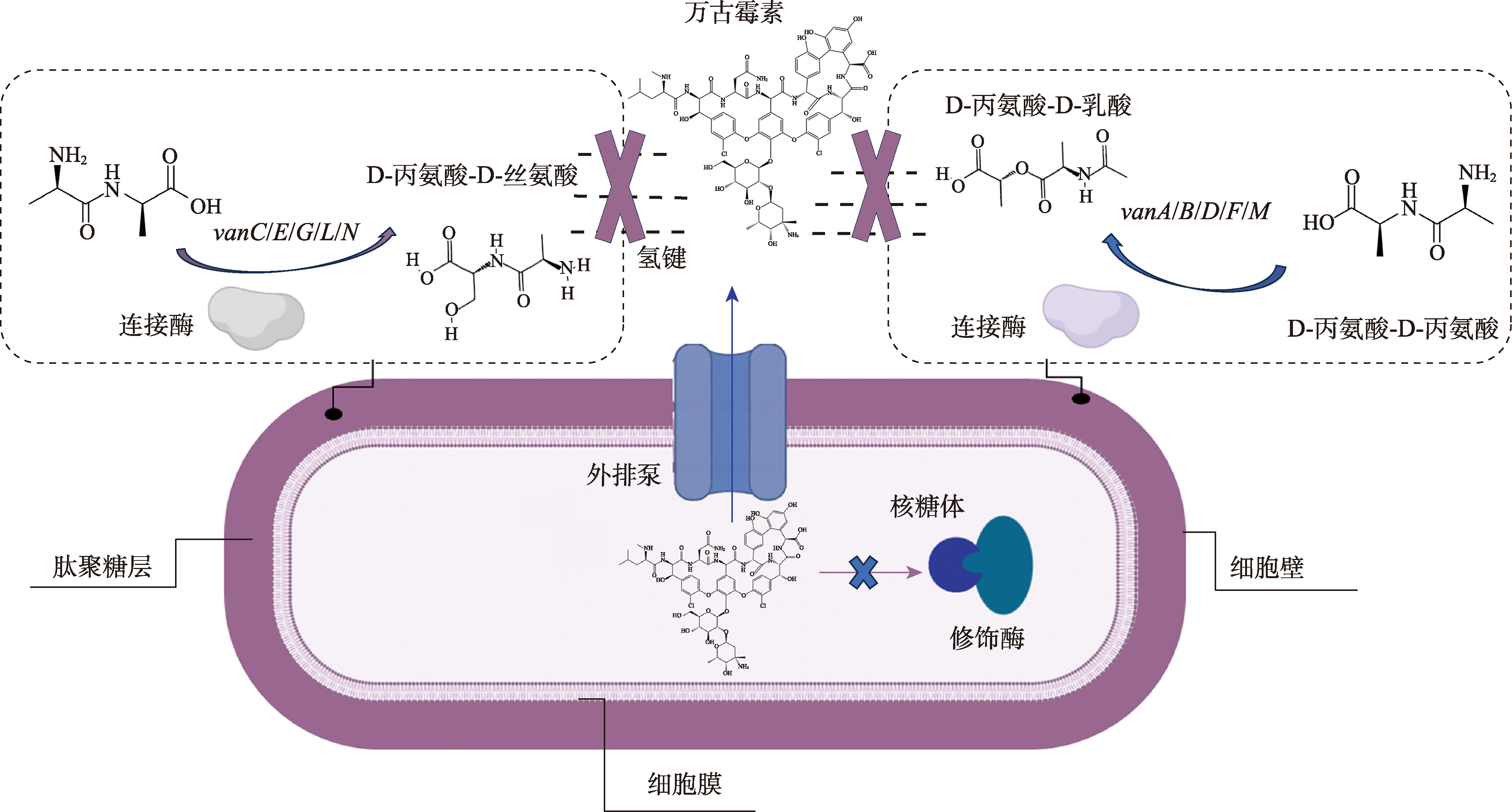
Progresses on the prevalence and mechanism of vancomycin- resistant bacteria
Yao Shen1,2,3( ), Zhiyu Li2, Fengcheng Miao2, Yingping Xiao3, Hua Yang2,3, Yali Dang1(
), Zhiyu Li2, Fengcheng Miao2, Yingping Xiao3, Hua Yang2,3, Yali Dang1( ), Jiangang Ma2(
), Jiangang Ma2( )
)
- 1. College of Food Science and Engineering, Ningbo University, Ningbo 315832, China
2. Xianghu Laboratory, Institute of Biotechnology, Hangzhou 311200, China
3. Institute of Quality, Safety and Nutrition of Agricultural Products, Zhejiang Academy of Agricultural Sciences, Hangzhou 310021, China
-
Received:2024-12-12Revised:2025-02-28Online:2025-06-20Published:2025-03-03 -
Contact:Yali Dang, Jiangang Ma E-mail:shenyao6267@163.com;dangyali@nbu.edu.cn;vetmajg@163.com -
Supported by:Program of Zhejiang Agriculture and Rural Affairs(2023SNJF062);Project of the Key Scientific and Technological Program of Hangzhou(2023SZD0058);China Agriculture Research System of MOF and MARA(CARS-42-27)
Cite this article
Yao Shen, Zhiyu Li, Fengcheng Miao, Yingping Xiao, Hua Yang, Yali Dang, Jiangang Ma. Progresses on the prevalence and mechanism of vancomycin- resistant bacteria[J]. Hereditas(Beijing), 2025, 47(6): 650-659.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
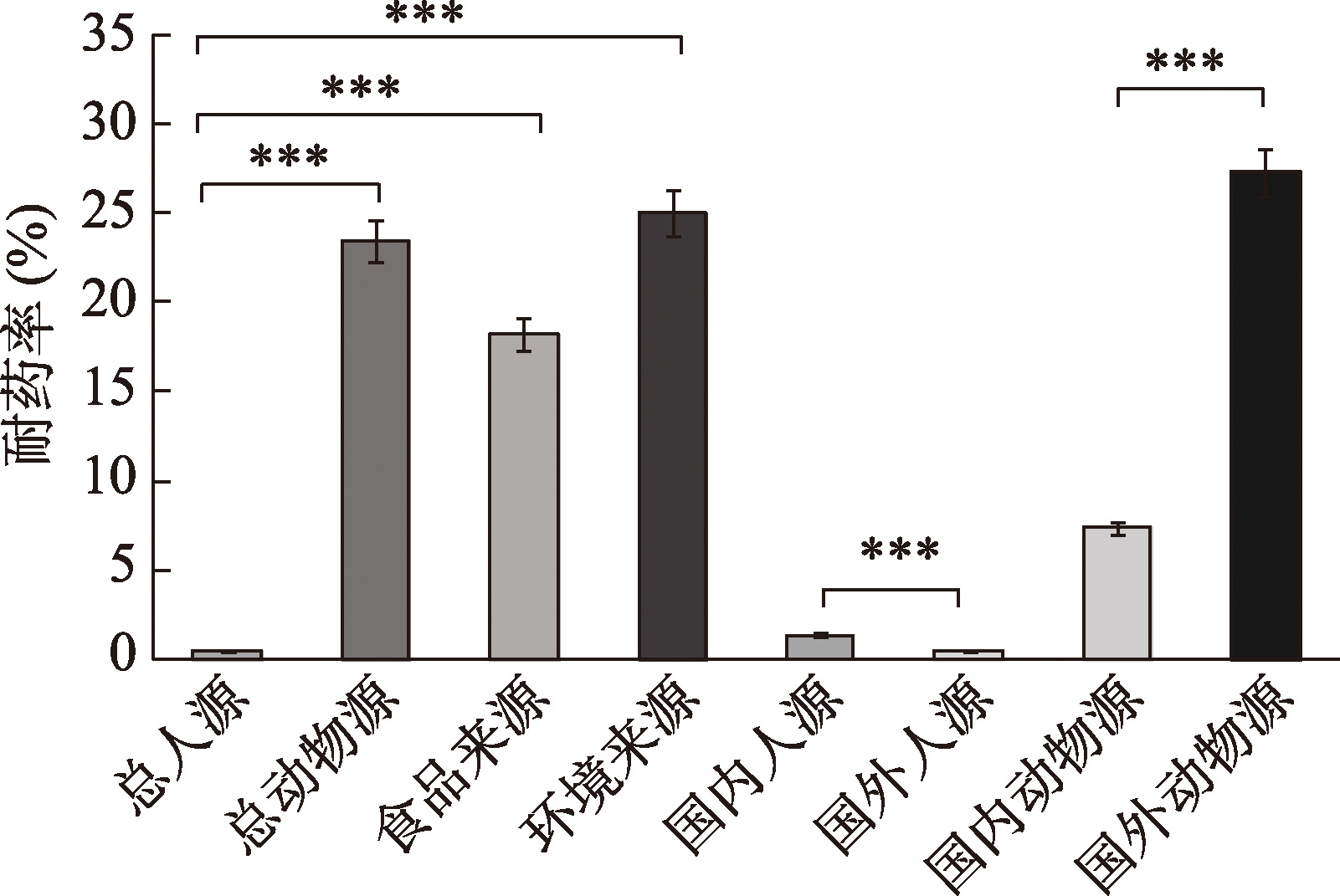
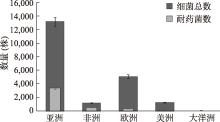
Table 1
Summary of the prevalence of drug-resistant bacteria from some different sources"
| 菌种类型 | 地区 | 年份(采样时间) | 耐药率(%) | 样本来源 | 参考文献 |
|---|---|---|---|---|---|
| 肠球菌 | 印度 | 2009* | 80.2 | 马 | [ |
| 意大利 | 2016* | 49 | 狗 | [ | |
| 中国甘肃 | 2020~2021 | 24.4 | 牛、羊、猪 | [ | |
| 中国北京 | 2015~2016 | 1.26 | 伴侣动物 | [ | |
| 欧洲 | 1996~2020* | 14.6 | 伴侣动物 | [ | |
| 南非 | 2011~2017 | 90.9 | 医院废水、地表水、地下水 | [ | |
| 捷克 | 2012~2013 | 86.48 | 医院废水处理植物 | [ | |
| 美国 | 2018* | 50 | 医院污水和城市污水 | [ | |
| 中国北京 | 2017 | 28.37 | 直肠拭子 | [ | |
| 埃及 | 2010~2022* | 50.86 | 临床样本 | [ | |
| 中国台湾 | 2010~2020 | 51.08 | 血流感染患者 | [ | |
| 金黄色葡萄球菌 | 埃及 | 2013~2014 | 5.5 | 临床样本和鼻拭子 | [ |
| 中国台湾 | 2012~2013 | 12.7 | 血液、脑脊液、腹水和胸腔积液 | [ | |
| 链球菌 | 马来西亚 | 2014~2015 | 100 | 牛肉 | [ |
| 艰难梭菌 | 全球 | 2007~2022* | 6.6 | 肉制品 | [ |
| 弧杆菌 | 伊朗 | 2012~2013 | 95.8 | 家禽肉 | [ |
| [1] |
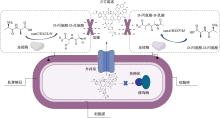
Li G, Walker MJ, De Oliveira DMP. Vancomycin resistance in Enterococcus and Staphylococcus aureus. Microorganisms, 2022, 11(1): 24.
pmid: 36677316 |
| [2] |
Howden BP, Davies JK, Johnson PDR, Stinear TP, Grayson ML. Reduced vancomycin susceptibility in Staphylococcus aureus, including vancomycin-intermediate and heterogeneous vancomycin-intermediate strains: resistance mechanisms, laboratory detection, and clinical implications. Clin Microbiol Rev, 2010, 23(1): 99-139.
pmid: 20065327 |
| [3] |
Selim S. Mechanisms of gram-positive vancomycin resistance (Review). Biomed Rep, 2022, 16(1): 7.
pmid: 34938536 |
| [4] |
Huang SH, Chen YC, Chuang YC, Chiu SK, Fung CP, Lu PL, Wang LS, Wu TL, Wang JT. Prevalence of vancomycin-intermediate Staphylococcus aureus (VISA) and heterogeneous VISA among methicillin-resistant S. aureus with high vancomycin minimal inhibitory concentrations in Taiwan: a multicenter surveillance study, 2012-2013. J Microbiol Immunol Infect, 2016, 49(5): 701-707.
pmid: 26320398 |
| [5] |
Tsai HY, Lee YL, Liu PY, Lu MC, Shao PL, Lu PL, Cheng SH, Ko WC, Lin CY, Wu TS, Yen MY, Wang LS, Liu CP, Lee WS, Shi ZY, Chen YS, Wang FD, Tseng SH, Chen YH, Sheng WH, Lee CM, Chen YH, Liao CH, Hsueh PR. Antimicrobial susceptibility of bacteremic vancomycin- resistant Enterococcus faecium to eravacycline, omadacycline, lipoglycopeptides, and other comparator antibiotics: results from the 2019-2020 nationwide surveillance of multicenter antimicrobial resistance in Taiwan (SMART). Int J Antimicrob Agents, 2021, 58(1): 106353.
pmid: 33961991 |
| [6] |
Yan MY, He YH, Ruan GJ, Xue F, Zheng B, Lv Y. The prevalence and molecular epidemiology of vancomycin- resistant Enterococcus (VRE) carriage in patients admitted to intensive care units in Beijing, China. J Microbiol Immunol Infect, 2023, 56(2): 351-357.
pmid: 35922268 |
| [7] |
Pfaller MA, Mendes RE, Streit JM, Hogan PA, Flamm RK. ZAAPS Program results for 2015: an activity and spectrum analysis of linezolid using clinical isolates from medical centres in 32 countries. J Antimicrob Chemother, 2017, 72(11): 3093-3099.
pmid: 28961701 |
| [8] |
Mendes RE, Deshpande L, Streit JM, Sader HS, Castanheira M, Hogan PA, Flamm RK. ZAAPS programme results for 2016: an activity and spectrum analysis of linezolid using clinical isolates from medical centres in 42 countries. J Antimicrob Chemother, 2018, 73(7): 1880-1887.
pmid: 29659858 |
| [9] |
Cimen C, Berends MS, Bathoorn E, Lokate M, Voss A, Friedrich AW, Glasner C, Hamprecht A. Vancomycin- resistant enterococci (VRE) in hospital settings across European borders: a scoping review comparing the epidemiology in the Netherlands and Germany. Antimicrob Resist Infect Control, 2023, 12(1): 78.
pmid: 37568229 |
| [10] |
Rödenbeck M, Ayobami O, Eckmanns T, Pletz MW, Bleidorn J, Markwart R. Clinical epidemiology and case fatality due to antimicrobial resistance in Germany: a systematic review and meta-analysis, 1 January 2010 to 31 December 2021. Euro Surveill, 2023, 28(20): 2200672.
pmid: 37199987 |
| [11] |
Kajihara T, Yahara K, Hirabayashi A, Shibayama K, Sugai M. Japan nosocomial infections surveillance (JANIS): current status, international collaboration, and future directions for a comprehensive antimicrobial resistance surveillance system. Jpn J Infect Dis, 2021, 74(2): 87-96.
pmid: 32863357 |
| [12] |
Azzam A, Elkafas H, Khaled H, Ashraf A, Yousef M, Elkashef AA. Prevalence of vancomycin-resistant enterococci (VRE) in Egypt (2010-2022): a systematic review and meta-analysis. J Egypt Public Health Assoc, 2023, 98(1): 8.
pmid: 37037955 |
| [13] |
Fridkin SK. Vancomycin-intermediate and -resistant Staphylococcus aureus: what the infectious disease specialist needs to know. Clin Infect Dis, 2001, 32(1): 108-115.
pmid: 11118389 |
| [14] |
Melese A, Genet C, Andualem T. Prevalence of vncomycin resistant enterococci (VRE) in Ethiopia: a systematic review and meta-analysis. BMC Infect Dis, 2020, 20(1): 124.
pmid: 32046668 |
| [15] | Bai YT, Kan W, Liu P, Yang XP. Isolation, identification and antibiotic resistance investigation of enterococcus from different livestock in parts of Gansu province. J Gansu Agric Univ, 2022, 57(6): 25-32. |
| 白亚彤, 阚威, 刘沛, 杨孝朴. 甘肃部分地区动物源肠球菌的分离鉴定及耐药性研究. 甘肃农业大学学报, 2022, 57(6): 25-32. | |
| [16] | Feng WW, Du XX, Cao BX, Liang B. Surveillance of antimicrobial resistance in five animal-derived enterococci. Heilongjiang Anim. Sci. Vet. Med, 2011, (9): 122-124. |
| 冯雯雯, 杜昕昕, 曹宾霞, 梁斌. 五种动物源肠球菌耐药性监测. 黑龙江畜牧兽医, 2011, (9): 122-124. | |
| [17] | Wu JR, Wu LY, Chen XG, Sun T, Liu C, Chen X, Hong J, Zhong Y, Luo XQ, Yu DG. Molecular typing through REP-PCR and detection of drug resistant of VRE isolated from different sources in safari park. Chin Vet Sci, 2018, 48(3): 395-402. |
| 吴家荣, 吴丽云, 陈晓刚, 孙彤, 刘灿, 陈荀, 洪娟, 钟艳, 罗小青, 俞道进. 野生动物园不同源性VRE耐药性及REP-PCR分型研究. 中国兽医科学, 2018, 48(3): 395-402. | |
| [18] | Wang HG, Yang DG, Gao SN, Ma HJ, Zhang JH, Shen JZ, Ding HL. Isolation, identification and drug sensitivity analysis of Staphylococcus aureus from animal farms in Chongqing. Chin J Vet Med, 2016, 52(9): 86-90. |
| 王豪举, 杨大吉, 高胜男, 马卉佳, 张家骅, 沈建忠, 丁红雷. 重庆市动物源性金黄色葡萄球菌的分离鉴定及药物敏感性分析. 中国兽医杂志, 2016, 52(9): 86-90. | |
| [19] |
Yu LP, Liu Y, Liu MD, Li ZX, Li L, Wang FK. Research note: molecular characterization of antimicrobial resistance and virulence gene analysis of Enterococcus faecalis in poultry in Tai'an, China. Poult Sci, 2022, 101(5): 101763.
pmid: 35263706 |
| [20] |
Singh BR. Prevalence of vancomycin resistance and multiple drug resistance in enterococci in equids in North India. J Infect Dev Ctries, 2009, 3(7): 498-503.
pmid: 19762967 |
| [21] | Pasotto D, Dotto G, Menandro ML, Mondin A, Martini M. Prevalence and antimicrobial-resistance characterization of vancomycin resistant enterococci (VRE) strains in healthy household dogs in Italy. Int J Infect Dis, 2016, 53: 50. |
| [22] |
Gonçalves A, Igrejas G, Radhouani H, López M, Guerra A, Petrucci-Fonseca F, Alcaide E, Zorrilla I, Serra R, Torres C, Poeta P. Detection of vancomycin-resistant enterococci from faecal samples of Iberian wolf and Iberian lynx, including Enterococcus faecium strains of CC17 and the new singleton ST573. Sci Total Environ, 2011, 410-411: 266-268.
pmid: 22018960 |
| [23] |
Thung TY, Radu S, Mahyudin NA, Rukayadi Y, Zakaria Z, Mazlan N, Tan BH, Lee E, Yeoh SL, Chin YZ, Tan CW, Kuan CH, Basri DF, Wan Mohamed Radzi CWJ. Prevalence, virulence genes and antimicrobial resistance profiles of Salmonella Serovars from retail beef in Selangor, Malaysia. Front Microbiol, 2018, 8: 2697.
pmid: 29379488 |
| [24] |
Tiwari A, Krolicka A, Tran TT, Räisänen K, Ásmundsdóttir ÁM, Wikmark OG, Lood R, Pitkänen T. Antibiotic resistance monitoring in wastewater in the Nordic countries: a systematic review. Environ Res, 2024, 246: 118052.
pmid: 38163547 |
| [25] |
Ateba CN, Lekoma KP, Kawadza DT. Detection of vanA and vanB genes in vancomycin-resistant enterococci (VRE) from groundwater using multiplex PCR analysis. J Water Health, 2013, 11(4): 684-691.
pmid: 24334842 |
| [26] |
Iweriebor BC, Gaqavu S, Obi LC, Nwodo UU, Okoh AI. Antibiotic susceptibilities of enterococcus species isolated from hospital and domestic wastewater effluents in alice, eastern cape province of South Africa. Int J Environ Res Public Health, 2015, 12(4): 4231-4246.
pmid: 25893999 |
| [27] |
Matlou DP, Bissong MEA, Tchatchouang CDK, Adem MR, Foka FET, Kumar A, Ateba CN. Virulence profiles of vancomycin-resistant enterococci isolated from surface and ground water utilized by humans in the North West province, South Africa: a public health perspective. Environ Sci Pollut Res Int, 2019, 26(15): 15105-15114.
pmid: 30924038 |
| [28] | Wu LY, Hong J, Sun T, Chen X, Liu C, Zhong Y, Xu YJ, Wang GS, Yu DJ. Study on resistance of water-borne Enterococcus to benzalkonium bromide and antibiotics. Chin Vet Sci, 2018, 48(11): 1406-1414. |
| 吴丽云, 洪娟, 孙彤, 陈荀, 刘灿, 钟艳, 许缘君, 王冠淞, 俞道进. 水源性肠球菌对苯扎溴铵及部分抗菌药的耐药性研究. 中国兽医科学, 2018, 48(11): 1406-1414. | |
| [29] | Chen X, Zhao XF, Bai XM, Che J, Zhang YF, Yuan M, Li J. Research on antimicrobial resistance characteristics of Enterococcus spp. from companion animals in Beijing. China Animal Husbandry and Veterinary Medicine, 2020, 47 (12): 4119-4126. |
| 陈霞, 赵晓菲, 白雪梅, 车洁, 张云飞, 袁敏, 李娟. 北京市伴侣动物源肠球菌的抗菌药物耐受情况调查. 中国畜牧兽医, 2020, 47 (12): 4119-4126. | |
| [30] |
Wada Y, Irekeola AA, E A R ENS, Yusof W, Lih Huey L, Ladan Muhammad S, Harun A, Yean CY, Zaidah AR. Prevalence of vancomycin-resistant Enterococcus (VRE) in companion animals: the first meta-analysis and systematic review. Antibiotics (Basel), 2021, 10(2): 138.
pmid: 33572528 |
| [31] |
Oravcova V, Mihalcin M, Zakova J, Pospisilova L, Masarikova M, Literak I. Vancomycin-resistant enterococci with vanA gene in treated municipal wastewater and their association with human hospital strains. Sci Total Environ, 2017, 609: 633-43.
pmid: 28763660 |
| [32] |
Basode VK, Abdulhaq A, Alamoudi MUA, Tohari HM, Quhal WA, Madkhali AM, Hobani YH, Hershan AA. Prevalence of a carbapenem-resistance gene (KPC), vancomycin-resistance genes (van A/B) and a methicillin- resistance gene (mecA) in hospital and municipal sewage in a southwestern province of Saudi Arabia. BMC Res Notes, 2018, 11(1): 30.
pmid: 29335025 |
| [33] |
Bender JK, Cattoir V, Hegstad K, Sadowy E, Coque TM, Westh H, Hammerum AM, Schaffer K, Burns K, Murchan S, Novais C, Freitas AR, Peixe L, Del Grosso M, Pantosti A, Werner G. Update on prevalence and mechanisms of resistance to linezolid, tigecycline and daptomycin in enterococci in Europe: towards a common nomenclature. Drug Resist Updat, 2018, 40: 25-39.
pmid: 30447411 |
| [34] |
Dungan RS, Bjorneberg DL. Antimicrobial resistance in Escherichia coli and Enterococcal isolates from irrigation return flows in a high-desert watershed. Front Microbiol, 2021, 12: 660697.
pmid: 34054760 |
| [35] |
Esfandiari Z, Shoaei P, Vakili B, Farajzadegan Z, Tarrahi MJ, Emami Z, Fakhri Y, Weese JS, Mahmudiono T. Prevalence and antibiotic resistance of Clostridioides (Clostridium difficile) In meat and meat products: a systematic review and meta-analysis. Iran J Public Health, 2023, 52(12): 2516-2527.
pmid: 38435778 |
| [36] |
Lytsy B, Engstrand L, Gustafsson Å, Kaden R. Time to review the gold standard for genotyping vancomycin- resistant enterococci in epidemiology: Comparing whole- genome sequencing with PFGE and MLST in three suspected outbreaks in Sweden during 2013-2015. Infect Genet Evol, 2017, 54: 74-80.
pmid: 28627467 |
| [37] | Li YS, Li XN, Han JZ, Gao D, Wu FJ. Monitoring and analysis of drug resistance of Enterococcus faecalis in northeast China. Modern Journal of Animal Husbandry and Veterinary Medicine, 2018, (2): 42-47. |
| 李延山, 李欣南, 韩镌竹, 高铎, 武凤娇. 东北地区动物源粪肠球菌耐药性监测与分析. 现代畜牧兽医, 2018, (2): 42-47. | |
| [38] | Tang B, Hao Y, Lin JH, Wang JG, Ji XF, Qian MR, Yang H. Comparison and analysis of antimicrobial resistance of Escherichia coli and Enterococcus isolated from animals in Jinhua city and Taizhou city of Zhejiang province. J Zhejiang Univ (Agric Life Sci), 2021, 47(5): 647-659. |
| 唐标, 郝运, 林家辉, 王静鸽, 吉小凤, 钱鸣蓉, 杨华. 浙江省2市动物源大肠埃希菌及肠球菌耐药性比较和分析. 浙江大学学报(农业与生命科学版), 2021, 47(5): 647-659. | |
| [39] | Ming Y, Qiu Y, Zhou JL, Tan RF, Wei GL, Xu RJ, Wu PF. Isolation and identification of Staphylococcus aureus from different animal sources and analysis of drug resistance. Heilongjiang Anim Sci Vet Med, 2020, (19): 101-106+ 172. |
| 明杨, 邱雨, 周杰珑, 谭瑞丰, 魏港利, 徐瑞娟, 吴培福. 不同动物源金黄色葡萄球菌的分离鉴定与耐药性分析. 黑龙江畜牧兽医, 2020, (19): 101-106+172. | |
| [40] | Chen CH, Xu XG. Genetic characteristics of vancomycin resistance gene cluster in Enterococcus spp. Hereditas (Beijing), 2015, 37(5): 452-457. |
| 陈春辉, 徐晓刚. 肠球菌万古霉素耐药基因簇遗传特性. 遗传, 2015, 37(5): 452-457. | |
| [41] |
Cong YG, Yang SJ, Rao XC. Vancomycin resistant Staphylococcus aureus infections: a review of case updating and clinical features. J Adv Res, 2019, 21: 169-176.
pmid: 32071785 |
| [42] |
Kankalil George S, Suseela MR, El Safi S, Ali Elnagi E, Al-Naam YA, Adlan Mohammed Adam A, Mary Jacob A, Al-Maqati T, Kumar Ks H. Molecular determination of van genes among clinical isolates of enterococci at a hospital setting. Saudi J Biol Sci, 2021, 28(5): 2895-2899.
pmid: 34012328 |
| [43] |
Cao RB, Su HM, Wei ZC, He ZE, Pan T, Li YJ, Sun BL. An induced mutation of ABC-transporter component VraF(K84E) contributes to vancomycin resistance and virulence in Staphylococcus aureus strain MW2. Int J Med Microbiol, 2024, 315: 151624.
pmid: 38838390 |
| [44] | Xu T, Huang HH. Progress on mechanisms of antibiotic resistance in Clostridioides difficile. Hereditas (Beijing), 2023, 45(11):1028-1038. |
| 胥腾, 黄海辉. 艰难梭菌抗菌药物耐药机制研究进展. 遗传, 2023, 45(11):1028-1038. | |
| [45] |
Meziane-Cherif D, Stogios PJ, Evdokimova E, Egorova O, Savchenko A, Courvalin P. Structural and functional adaptation of vancomycin resistance VanT serine racemases. mBio, 2015, 6(4): e00806.
pmid: 26265719 |
| [46] |
De Oliveira DMP, Forde BM, Kidd TJ, Harris PNA, Schembri MA, Beatson SA, Paterson DL, Walker MJ. Antimicrobial resistance in ESKAPE pathogens. Clin Microbiol Rev, 2020, 33(3): e00181-19.
pmid: 32404435 |
| [47] |
Gill SR, Fouts DE, Archer GL, Mongodin EF, Deboy RT, Ravel J, Paulsen IT, Kolonay JF, Brinkac L, Beanan M, Dodson RJ, Daugherty SC, Madupu R, Angiuoli SV, Durkin AS, Haft DH, Vamathevan J, Khouri H, Utterback T, Lee C, Dimitrov G, Jiang LX, Qin HY, Weidman J, Tran K, Kang K, Hance IR, Nelson KE, Fraser CM. Insights on evolution of virulence and resistance from the complete genome analysis of an early methicillin-resistant Staphylococcus aureus strain and a biofilm-producing methicillin-resistant Staphylococcus epidermidis strain. J Bacteriol, 2005, 187(7): 2426-2438.
pmid: 15774886 |
| [48] |
Terra MR, Tosoni NF, Furlaneto MC, Furlaneto-Maia L. Assessment of vancomycin resistance transfer among enterococci of clinical importance in milk matrix. J Environ Sci Health B, 2019, 54(12): 925-929.
pmid: 31382830 |
| [49] |
Skowron K, Jeleńska A, Paluszak Z, Szala B. Prevalence and distribution of VRE (vancomycin resistant enterococci) and VSE (vancomycin susceptible enterococci) strains in the breeding environment. Ann Agric Environ Med, 2016, 23(2): 231-236.
pmid: 27294624 |
| [50] |
Hou ZR, Liu L, Wei JH, Xu BJ. Progress in the prevalence, classification and drug resistance mechanisms of methicillin-resistant Staphylococcus aureus. Infect Drug Resist, 2023, 16: 3271-3292.
pmid: 37255882 |
| [51] |
Islam M, Sharon B, Abaragu A, Sistu H, Akins RL, Palmer K. Vancomycin resistance in Enterococcus faecium from the Dallas, Texas, Area is conferred predominantly on pRUM-Likeplasmids. mSphere, 2023, 8(2): e0002423.
pmid: 36939336 |
| [52] |
Hammerum AM. Enterococci of animal origin and their significance for public health. Clin Microbiol Infect, 2012, 18(7): 619-625.
pmid: 22487203 |
| [53] |
Weaver KE. Enterococcal genetics. Microbiol Spectr, 2019, 7(2).
pmid: 30848235 |
| [54] |
Wardal E, Żabicka D, Skalski T, Kubiak-Pulkowska J, Hryniewicz W, Sadowy E. Characterization of a tigecycline-, linezolid- and vancomycin-resistant clinical Enteroccoccus faecium isolate, carrying vanA and vanB genes. Infect Dis Ther, 2023, 12(11): 2545-2565.
pmid: 37821741 |
| [55] |
Lehmkuhl J, Schneider JS, Werth KLV, Scherff N, Mellmann A, Kampmeier S. Role of membrane vesicles in the transmission of vancomycin resistance in Enterococcus faecium. Sci Rep, 2024, 14(1): 1895.
pmid: 38253607 |
| [56] |
Asadpour L, Ghazanfari N. Detection of vancomycin nonsusceptible strains in clinical isolates of Staphylococcus aureus in northern Iran. Int Microbiol, 2019, 22(4): 411-417.
pmid: 30811005 |
| [57] |
Stogios PJ, Savchenko A. Molecular mechanisms of vancomycin resistance. Protein Sci, 2020, 29(3): 654-669.
pmid: 31899563 |
| [58] |
Lebreton F, Depardieu F, Bourdon N, Fines-Guyon M, Berger P, Camiade S, Leclercq R, Courvalin P, Cattoir V. D-Ala-d-Ser VanN-type transferable vancomycin resistance in Enterococcus faecium. Antimicrob Agents Chemother, 2011, 55(10): 4606-4612.
pmid: 21807981 |
| [59] |
Périchon B, Courvalin P. VanA-type vancomycin-resistant Staphylococcus aureus. Antimicrob Agents Chemother, 2009, 53(11): 4580-4587.
pmid: 19506057 |
| [60] |
Girijan SK, Pillai D. Identification and characterization of vancomycin-resistant Staphylococcus aureus in hospital wastewaters: evidence of horizontal spread of antimicrobial resistance. J Water Health, 2021, 19(5): 785-795.
pmid: 34665771 |
| [61] |
Gousia P, Economou V, Bozidis P, Papadopoulou C. Vancomycin-resistance phenotypes, vancomycin-resistance genes, and resistance to antibiotics of enterococci isolated from food of animal origin. Foodborne Pathog Dis, 2015, 12(3): 214-220.
pmid: 25562594 |
| [62] |
Sparo M, Delpech G, García Allende N. Impact on public health of the spread of high-level resistance to gentamicin and vancomycin in Enterococci. Front Microbiol, 2018, 9: 3073.
pmid: 30619158 |
| No related articles found! |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||