Hereditas(Beijing) ›› 2022, Vol. 44 ›› Issue (10): 840-852.doi: 10.16288/j.yczz.22-265
• Review • Previous Articles Next Articles
Molecular mechanism of islet β-cell functional alternations during type 2 diabetes
Chengan Lv1,2( ), Ruoran Wang1,2, Zhuo-Xian Meng1,2(
), Ruoran Wang1,2, Zhuo-Xian Meng1,2( )
)
- 1. Department of Pathology and Pathophysiology, Zhejiang University School of Medicine, Hangzhou 310058, China
2. Key Laboratory of Disease Proteomics of Zhejiang Province, Zhejiang University School of Medicine, Hangzhou 310058, China
-
Received:2022-08-04Revised:2022-09-02Online:2022-10-20Published:2022-09-30 -
Contact:Meng Zhuo-Xian E-mail:3190100992@zju.edu.cn;zxmeng@zju.edu.cn -
Supported by:the National Natural Science Foundation of China(91857110);the National Natural Science Foundation of China(81722012);the National Natural Science Foundation of China(81670740);the National Key R&D Program of the Ministry of Science and Technology(2018YFA0800403);the National Key R&D Program of the Ministry of Science and Technology(2021YFC20701903);the Zhejiang Provincial Natural Science Foundation of China(LZ21H070001);the Construction Fund of Medical Key Disciplines of Hangzhou(OO20200055)
Cite this article
Chengan Lv, Ruoran Wang, Zhuo-Xian Meng. Molecular mechanism of islet β-cell functional alternations during type 2 diabetes[J]. Hereditas(Beijing), 2022, 44(10): 840-852.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
| [1] |
Association AD.2. Classification and diagnosis of diabetes: Standards of medical care in diabetes—2021. Diabetes Care, 2020, 44(Suppl 1): S15-S33.
doi: 10.2337/dc21-S002 |
| [2] | DeFronzo RA, Ferrannini E, Groop L, Henry RR, Herman WH, Holst JJ, Hu FB, Kahn CR, Raz I, Shulman GI, Simonson DC, Testa MA, Weiss R. Type 2 diabetes mellitus. Nat Rev Dis Primers, 2015, 115019. |
| [3] |
Chiou J, Zeng C, Cheng Z, Han JY, Schlichting M, Miller M, Mendez R, Huang S, Wang JZ, Sui YH, Deogaygay A, Okino ML, Qiu YJ, Sun Y, Kudtarkar P, Fang RX, Preissl S, Sander M, Gorkin DU, Gaulton KJ. Single-cell chromatin accessibility identifies pancreatic islet cell type- and state-specific regulatory programs of diabetes risk. Nat Genet, 2021, 53(4): 455-466.
doi: 10.1038/s41588-021-00823-0 pmid: 33795864 |
| [4] |
Krentz NAJ, Gloyn AL. Insights into pancreatic islet cell dysfunction from type 2 diabetes mellitus genetics. Nat Rev Endocrinol, 2020, 16(4): 202-212.
doi: 10.1038/s41574-020-0325-0 pmid: 32099086 |
| [5] |
Hudish LI, Reusch JE, Sussel L. Beta cell dysfunction during progression of metabolic syndrome to type 2 diabetes. J Clin Invest, 2019, 129(10): 4001-4008.
doi: 10.1172/JCI129188 pmid: 31424428 |
| [6] |
Hou J, Li Z, Zhong W, Hao Q, Lei L, Wang L, Zhao D, Xu P, Zhou Y, Wang Y, Xu T. Temporal transcriptomic and proteomic landscapes of deteriorating pancreatic islets in type 2 diabetic rats. Diabetes, 2017, 66(8): 2188-2200.
doi: 10.2337/db16-1305 pmid: 28559245 |
| [7] |
Wang RR, Qiu XY, Pan R, Fu HX, Zhang ZY, Wang QT, Chen HD, Wu QQ, Pan XW, Zhou YP, Shan PF, Wang SS, Guo GJ, Zheng M, Zhu LY, Meng ZX. Dietary intervention preserves beta cell function in mice through ctcf- mediated transcriptional reprogramming. J Exp Med, 2022, 219(7): e20211779.
doi: 10.1084/jem.20211779 |
| [8] |
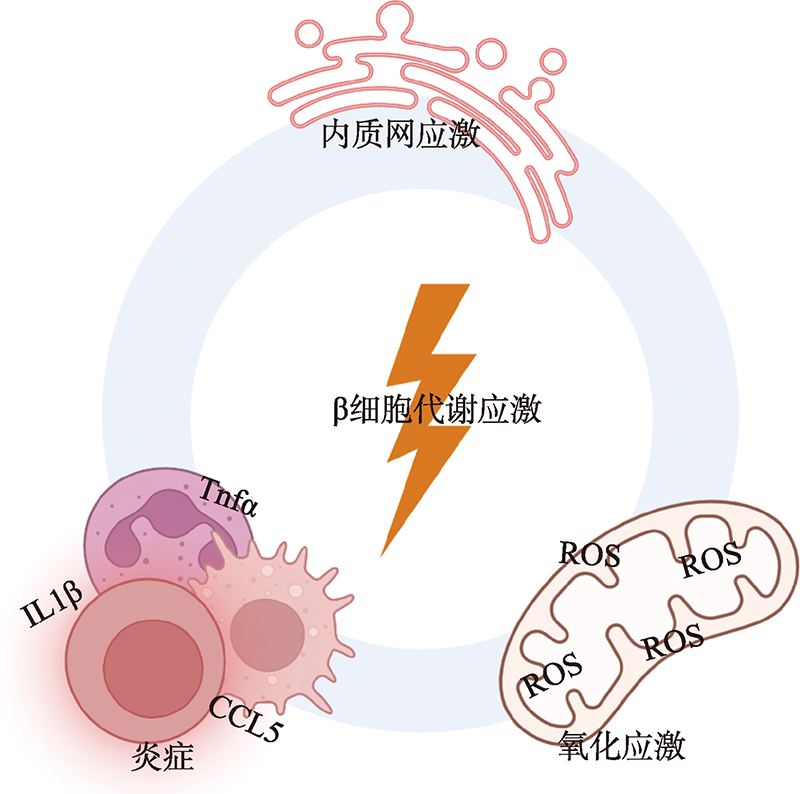
Prentki M, Nolan CJ. Islet beta cell failure in type 2 diabetes. J Clin Invest, 2006, 116(7): 1802-1812.
pmid: 16823478 |
| [9] |
Zhang ZY, Gao Y, Meng ZX. Transcriptional control of pancreatic beta-cell identity and plasticity during the pathogenesis of type 2 diabetes. J Genet Genomics, 2022, 49(4): 316-328.
doi: 10.1016/j.jgg.2022.03.002 |
| [10] | Fu Z, Gilbert ER, Liu DM. Regulation of insulin synthesis and secretion and pancreatic beta-cell dysfunction in diabetes. Curr Diabetes Rev, 2014, 9(1): 25-53 |
| [11] |
Campbell JE, Newgard CB. Mechanisms controlling pancreatic islet cell function in insulin secretion. Nat Rev Mol Cell Biol, 2021, 22(2): 142-158.
doi: 10.1038/s41580-020-00317-7 |
| [12] | Jewell JL, Russell RC, Guan KL. Amino acid signalling upstream of mTOR. Nat Rev Mol Cell Biol, 2013, 14(3): 133-139. |
| [13] |
Zhang X, Wang XW, Yuan ZQ, Radford SJ, Liu C, Libutti SK, Zheng XFS. Amino acids-RAB1a-mTORC1 signaling controls whole-body glucose homeostasis. Cell Rep, 2021, 34(11): 108830.
doi: 10.1016/j.celrep.2021.108830 |
| [14] |
Ferdaoussi M, Bergeron V, Zarrouki B, Kolic J, Cantley J, Fielitz J, Olson EN, Prentki M, Biden T, MacDonald PE, Poitout V.G protein-coupled receptor (GPR)40-dependent potentiation of insulin secretion in mouse islets is mediated by protein kinase D1. Diabetologia, 2012, 55(10): 2682-2692.
doi: 10.1007/s00125-012-2650-x pmid: 22820510 |
| [15] |
Itoh Y, Kawamata Y, Harada M, Kobayashi M, Fujii R, Fukusumi S, Ogi K, Hosoya M, Tanaka Y, Uejima H, Tanaka H, Maruyama M, Satoh R, Okubo S, Kizawa H, Komatsu H, Matsumura F, Noguchi Y, Shinobara T, Hinuma S, Fujisawa Y, Fujino M.Free fatty acids regulate insulin secretion from pancreatic beta cells through gpr40. Nature, 2003, 422(6928): 173-176.
doi: 10.1038/nature01478 |
| [16] |
Andersen A, Lund A, Knop FK, Vilsbøll T. Glucagon-like peptide1 in health and disease. Nat Rev Endocrinol, 2018, 14(7): 390-403.
doi: 10.1038/s41574-018-0016-2 pmid: 29728598 |
| [17] |
Holz GG. Epac: a new camp-binding protein in support of glucagon-like peptide-1 receptor-mediated signal transduction in the pancreatic beta-cell. Diabetes, 2004, 53(1): 5-13.
pmid: 14693691 |
| [18] |
Kashima Y, Miki T, Shibasaki T, Ozaki N, Miyazaki M, Yano H, Seino S. Critical role of camp-gefii—rim2 complex in incretin-potentiated insulin secretion. J Biol Chem, 2001, 276(49): 46046-46053.
doi: 10.1074/jbc.M108378200 pmid: 11598134 |
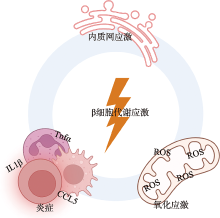
| [19] |
Ozaki N, Shibasaki T, Kashima Y, Miki T, Takahashi K, Ueno H, Sunaga Y, Yano H, Matsuura Y, Iwanaga T, Takai Y, Seino S. Camp-gefii is a direct target of camp in regulated exocytosis. Nat Cell Biol, 2000, 2(11): 805-811.
pmid: 11056535 |
| [20] |
Leibiger IB, Leibiger B, Berggren PO. Insulin signaling in the pancreatic beta-cell. Annu Rev Nutr, 2008, 28: 233-251.
doi: 10.1146/annurev.nutr.28.061807.155530 pmid: 18481923 |
| [21] |
Leibiger IB, Leibiger B, Moede T, Berggren PO. Exocytosis of insulin promotes insulin gene transcription via the insulin receptor/PI-3 kinase/p70 s6 kinase and cam kinase pathways. Mol Cell, 1998, 1(6): 933-938.
pmid: 9660977 |
| [22] |
Ansarullah, Jain C, Far FF, Homberg S, Wißmiller K, von Hahn FG, Raducanu A, Schirge S, Sterr M, Bilekova S, Siehler J, Wiener J, Oppenländer L, Morshedi A, Bastidas-Ponce A, Collden G, Irmler M, Beckers J, Feuchtinger A, Grzybek M, Ahlbrecht C, Feederle R, Plettenburg O, Müller TD, Meier M, Tschöp MH, Coskun Ü, Lickert H,. Inceptor counteracts insulin signalling in β-cells to control glycaemia. Nature, 2021, 590(7845): 326-331.
doi: 10.1038/s41586-021-03225-8 |
| [23] |
Qin JJ, Li YR, Cai ZM, Li SH, Zhu JF, Zhang F, Liang SS, Zhang WW, Guan YL, Shen DQ, Peng YQ, Zhang DY, Jie ZY, Wu WX, Qin YW, Xue WB, Li JH, Han LC, Lu DH, Wu PX, Dai YL, Sun XJ, Li ZS, Tang AF, Zhong SL, Li XP, Chen WN, Xu R, Wang MB, Feng Q, Gong MH, Yu J, Zhang YY, Zhang M, Hansen T, Sanchez G, Raes J, Falony G, Okuda S, Almeida M, LeChatelier E, Renault P, Pons N, Batto JM, Zhang ZX, Chen H, Yang RF, Zheng WM, Li SG, Yang HM, Wang J, Ehrlich SD, Nielsen R, Pedersen O, Kristiansen K, Wang J. A metagenome-wide association study of gut microbiota in type 2 diabetes. Nature, 2012, 490(7418): 55-60.
doi: 10.1038/nature11450 |
| [24] |
Tremaroli V, Bäckhed F. Functional interactions between the gut microbiota and host metabolism. Nature, 2012, 489(7415): 242-249.
doi: 10.1038/nature11552 |
| [25] |
Zhang Q, Pan Y, Zeng BH, Zheng XJ, Wang HF, Shen XY, Li H, Jiang Q, Zhao JX, Meng ZX, Li PP, Chen ZJ, Wei H, Liu ZH. Intestinal lysozyme liberates Nod1 ligands from microbes to direct insulin trafficking in pancreatic beta cells. Cell Res, 2019, 29(7): 516-532.
doi: 10.1038/s41422-019-0190-3 pmid: 31201384 |
| [26] |
Zhao LP, Zhang F, Ding XY, Wu GJ, Lam YY, Wang XJ, Fu HQ, Xue XH, Lu CH, Ma JL, Yu LH, Xu CM, Ren ZY, Xu Y, Xu SM, Shen HL, Zhu XL, Shi Y, Shen QY, Dong WP, Liu R, Ling YX, Zeng Y, Wang XP, Zhang QP, Wang J, Wang LH, Wu YQ, Zeng BH, Wei H, Zhang MH, Peng YD, Zhang CH. Gut bacteria selectively promoted by dietary fibers alleviate type 2 diabetes. Science, 2018, 359(6380): 1151-1156.
doi: 10.1126/science.aao5774 pmid: 29590046 |
| [27] |
Perry RJ, Peng L, Barry NA, Cline GW, Zhang DY, Cardone RL, Petersen KF, Kibbey RG, Goodman AL, Shulman GI. Acetate mediates a microbiome-brain-β-cell axis to promote metabolic syndrome. Nature, 2016, 534(7606): 213-217.
doi: 10.1038/nature18309 |
| [28] |
Hill JH, Franzosa EA, Huttenhower C, Guillemin K. A conserved bacterial protein induces pancreatic beta cell expansion during zebrafish development. eLife, 2016, 5: e20145.
doi: 10.7554/eLife.20145 |
| [29] |
Almaça J, Caicedo A, Landsman L. Beta cell dysfunction in diabetes: The islet microenvironment as an unusual suspect. Diabetologia, 2020, 63(10): 2076-2085.
doi: 10.1007/s00125-020-05186-5 pmid: 32894318 |
| [30] |
Huising MO. Paracrine regulation of insulin secretion. Diabetologia, 2020, 63(10): 2057-2063.
doi: 10.1007/s00125-020-05213-5 pmid: 32894316 |
| [31] |
Zhang X, Luo SY, Wang MJ, Huang Q, Fang WQ, Li J, Liu TX, Zhang YY, Deng ZY, Liu CL, Guan SL, Ayala JE, Flavell RA, Kulkarni RN, Libby P, Guo JL, Liu ZS, Shi GP. IL 18 signaling causes islet β cell development and insulin secretion via different receptors on acinar and β cells. Dev Cell, 2022, 57(12): 1496-1511.e1496.
doi: 10.1016/j.devcel.2022.05.013 pmid: 35675813 |
| [32] |
Dror E, Dalmas E, Meier DT, Wueest S, Thévenet J, Thienel C, Timper K, Nordmann TM, Traub S, Schulze F, Item F, Vallois D, Pattou F, Kerr-Conte J, Lavallard V, Berney T, Thorens B, Konrad D, Böni-Schnetzler M, Donath MY. Postprandial macrophage-derived IL-1β stimulates insulin, and both synergistically promote glucose disposal and inflammation. Nat Immunol, 2017, 18(3): 283-292.
doi: 10.1038/ni.3659 pmid: 28092375 |
| [33] |
Thorens B. Neural regulation of pancreatic islet cell mass and function. Diabetes Obes Metab, 2014, 16(Suppl 1): 87-95.
doi: 10.1111/dom.12346 |
| [34] |
Gilon P, Henquin JC. Mechanisms and physiological significance of the cholinergic control of pancreatic beta-cell function. Endocr Rev, 2001, 22(5): 565-604.
pmid: 11588141 |
| [35] |
Rosengren AH, Jokubka R, Tojjar D, Granhall C, Hansson O, Li DQ, Nagaraj V, Reinbothe TM, Tuncel J, Eliasson L, Groop L, Rorsman P, Salehi A, Lyssenko V, Luthman H, Renström E. Overexpression of alpha2A- adrenergic receptors contributes to type 2 diabetes. Science, 2010, 327(5962): 217-220.
doi: 10.1126/science.1176827 pmid: 19965390 |
| [36] |
Lv CA, Sun YC, Zhang ZY, Aboelela Z, Qiu XY, Meng ZX. β-cell dynamics in type 2 diabetes and in dietary and exercise interventions. J Mol Cell Biol, 2022, doi: 10.1093/jmcb/mjac046.
doi: 10.1093/jmcb/mjac046 |
| [37] |
Thorel F, Népote V, Avril I, Kohno K, Desgraz R, Chera S, Herrera PL. Conversion of adult pancreatic alpha-cells to beta-cells after extreme beta-cell loss. Nature, 2010, 464(7292): 1149-1154.
doi: 10.1038/nature08894 |
| [38] |
Chera S, Baronnier D, Ghila L, Cigliola V, Jensen JN, Gu G, Furuyama K, Thorel F, Gribble FM, Reimann F, Herrera PL. Diabetes recovery by age-dependent conversion of pancreatic δ-cells into insulin producers. Nature, 2014, 514(7523): 503-507.
doi: 10.1038/nature13633 |
| [39] |
Gribben C, Lambert C, Messal HA, Hubber EL, Rackham C, Evans I, Heimberg H, Jones P, Sancho R, Behrens A. Ductal Ngn3-expressing progenitors contribute to adult β cell neogenesis in the pancreas. Cell Stem Cell, 2021, 28(11): 2000-2008.e2004.
doi: 10.1016/j.stem.2021.08.003 pmid: 34478642 |
| [40] |
Zhao H, Huang XZ, Liu ZX, Pu WJ, Lv Z, He LJ, Li Y, Zhou Q, Lui KO, Zhou B. Pre-existing beta cells but not progenitors contribute to new beta cells in the adult pancreas. Nat Metab, 2021, 3(3): 352-365.
doi: 10.1038/s42255-021-00364-0 pmid: 33723463 |
| [41] |
Zhang HJ, Zhang J, Pope CF, Crawford LA, Vasavada RC, Jagasia SM, Gannon M. Gestational diabetes mellitus resulting from impaired beta-cell compensation in the absence of FoxM1, a novel downstream effector of placental lactogen. Diabetes, 2010, 59(1): 143-152.
doi: 10.2337/db09-0050 pmid: 19833884 |
| [42] |
Cerf ME. High fat programming of beta cell compensation, exhaustion, death and dysfunction. Pediatr Diabetes, 2015, 16(2): 71-78.
doi: 10.1111/pedi.12137 pmid: 25682938 |
| [43] |
Eizirik DL, Cardozo AK, Cnop M. The role for endoplasmic reticulum stress in diabetes mellitus. Endocr Rev, 2008, 29(1): 42-61.
doi: 10.1210/er.2007-0015 pmid: 18048764 |
| [44] |
Nordmann TM, Dror E, Schulze F, Traub S, Berishvili E, Barbieux C, Böni-Schnetzler M, Donath MY. The role of inflammation in β-cell dedifferentiation. Sci Rep, 2017, 7(1): 6285.
doi: 10.1038/s41598-017-06731-w pmid: 28740254 |
| [45] | Defronzo RA.Banting Lecture. From the triumvirate to the ominous octet:a new paradigm for the treatment of type 2 diabetes mellitus. Diabetes, 2009, 58(4): 773-795. |
| [46] |
Ozcan U, Yilmaz E, Ozcan L, Furuhashi M, Vaillancourt E, Smith RO, Görgün CZ, Hotamisligil GS. Chemical chaperones reduce ER stress and restore glucose homeostasis in a mouse model of type 2 diabetes. Science, 2006, 313(5790): 1137-1140.
doi: 10.1126/science.1128294 pmid: 16931765 |
| [47] |
Bensellam M, Laybutt DR, Jonas JC. The molecular mechanisms of pancreatic β-cell glucotoxicity: recent findings and future research directions. Mol Cell Endocrinol, 2012, 364(1-2): 1-27.
doi: 10.1016/j.mce.2012.08.003 pmid: 22885162 |
| [48] |
Kharroubi I, Ladrière L, Cardozo AK, Dogusan Z, Cnop M, Eizirik DL. Free fatty acids and cytokines induce pancreatic beta-cell apoptosis by different mechanisms: role of nuclear factor-kappaB and endoplasmic reticulum stress. Endocrinology, 2004, 145(11): 5087-5096.
doi: 10.1210/en.2004-0478 pmid: 15297438 |
| [49] |
Cnop M, Ladriere L, Hekerman P, Ortis F, Cardozo AK, Dogusan Z, Flamez D, Boyce M, Yuan J, Eizirik DL. Selective inhibition of eukaryotic translation initiation factor 2 alpha dephosphorylation potentiates fatty acid-induced endoplasmic reticulum stress and causes pancreatic beta-cell dysfunction and apoptosis. J Biol Chem, 2007, 282(6): 3989-3997.
doi: 10.1074/jbc.M607627200 pmid: 17158450 |
| [50] |
Preston AM, Gurisik E, Bartley C, Laybutt DR, Biden TJ. Reduced endoplasmic reticulum (ER)-to-Golgi protein trafficking contributes to ER stress in lipotoxic mouse beta cells by promoting protein overload. Diabetologia, 2009, 52(11): 2369-2373.
doi: 10.1007/s00125-009-1506-5 pmid: 19727664 |
| [51] |
Pétremand J, Puyal J, Chatton JY, Duprez J, Allagnat F, Frias M, James RW, Waeber G, Jonas JC, Widmann C. HDLs protect pancreatic β-cells against ER stress by restoring protein folding and trafficking. Diabetes, 2012, 61(5): 1100-1111.
doi: 10.2337/db11-1221 pmid: 22399686 |
| [52] |
Jeffrey KD, Alejandro EU, Luciani DS, Kalynyak TB, Hu XK, Li H, Lin YL, Townsend RR, Polonsky KS, Johnson JD. Carboxypeptidase E mediates palmitate-induced beta-cell ER stress and apoptosis. Proc Natl Acad Sci USA, 2008, 105(24): 8452-8457.
doi: 10.1073/pnas.0711232105 |
| [53] |
Huang CJ, Lin CY, Haataja L, Gurlo T, Butler AE, Rizza RA, Butler PC. High expression rates of human islet amyloid polypeptide induce endoplasmic reticulum stress mediated beta-cell apoptosis, a characteristic of humans with type 2 but not type 1 diabetes. Diabetes, 2007, 56(8): 2016-2027.
doi: 10.2337/db07-0197 |
| [54] |
Yamamoto WR, Bone RN, Sohn P, Syed F, Reissaus CA, Mosley AL, Wijeratne AB, True JD, Tong X, Kono T, Evans-Molina C. Endoplasmic reticulum stress alters ryanodine receptor function in the murine pancreatic beta cell. J Biol Chem, 2019, 294(1): 168-181.
doi: 10.1074/jbc.RA118.005683 pmid: 30420428 |
| [55] |
Hetz C. The unfolded protein response: controlling cell fate decisions under ER stress and beyond. Nat Rev Mol Cell Biol, 2012, 13(2): 89-102.
doi: 10.1038/nrm3270 |
| [56] |
Harding HP, Novoa I, Zhang Y, Zeng H, Wek R, Schapira M, Ron D. Regulated translation initiation controls stress-induced gene expression in mammalian cells. Mol Cell, 2000, 6(5): 1099-1108.
doi: 10.1016/s1097-2765(00)00108-8 pmid: 11106749 |
| [57] |
Hollien J, Weissman JS. Decay of endoplasmic reticulum- localized mRNAs during the unfolded protein response. Science, 2006, 313(5783): 104-107.
pmid: 16825573 |
| [58] |
Kroemer G, Mariño G, Levine B. Autophagy and the integrated stress response. Mol Cell, 2010, 40(2): 280-293.
doi: 10.1016/j.molcel.2010.09.023 pmid: 20965422 |
| [59] |
Lee AH, Chu GC, Iwakoshi NN, Glimcher LH. XBP-1 is required for biogenesis of cellular secretory machinery of exocrine glands. EMBO J, 2005, 24(24): 4368-4380.
doi: 10.1038/sj.emboj.7600903 |
| [60] |
Huang H, Yang KY, Wang RN, Han WH, Kuny S, Horn P, Zelmanovitz, Sauvé Y, Chan CB. β-Cell compensation concomitant with adaptive endoplasmic reticulum stress and β-cell neogenesis in a diet-induced type 2 diabetes model. Appl Physiol Nutr Metab, 2019, 44(12): 1355-1366.
doi: 10.1139/apnm-2019-0144 pmid: 31082326 |
| [61] |
Hwang JW, Qi L. Quality control in the endoplasmic reticulum: crosstalk between ERAD and UPR pathways. Trends Biochem Sci, 2018, 43(8): 593-605.
doi: S0968-0004(18)30122-1 pmid: 30056836 |
| [62] |
Xu TF, Yang L, Yan C, Wang XX, Huang P, Zhao F, Zhao LY, Zhang ML, Jia WP, Wang XD, Liu Y. The IRE1α- XBP1 pathway regulates metabolic stress-induced compensatory proliferation of pancreatic β-cells. Cell Res, 2014, 24(9): 1137-1140.
doi: 10.1038/cr.2014.55 |
| [63] |
Sharma RB, O'Donnell AC, Stamateris RE, Ha B, McCloskey KM, Reynolds PR, Arvan P, Alonso LC. Insulin demand regulates β cell number via the unfolded protein response. J Clin Invest, 2015, 125(10): 3831-3846.
doi: 10.1172/JCI79264 pmid: 26389675 |
| [64] |
Burgos-Morón E, Abad-Jiménez Z, Marañón AM, Iannantuoni F, Escribano-López I, López-Domènech S, Salom C, Jover A, Mora V, Roldan I, Solá E, Rocha M, Víctor VM. Relationship between oxidative stress, ER stress, and inflammation in type 2 diabetes: the battle continues. J Clin Med, 2019, 8(9): 1385.
doi: 10.3390/jcm8091385 |
| [65] |
Bae YS, Oh H, Rhee SG, Yoo YD. Regulation of reactive oxygen species generation in cell signaling. Mol Cells, 2011, 32(6): 491-509.
doi: 10.1007/s10059-011-0276-3 pmid: 22207195 |
| [66] |
Sekine N, Cirulli V, Regazzi R, Brown LJ, Gine E, Tamarit-Rodriguez J, Girotti M, Marie S, MacDonald MJ, Wollheim CB. Low lactate dehydrogenase and high mitochondrial glycerol phosphate dehydrogenase in pancreatic beta-cells. Potential role in nutrient sensing. J Biol Chem, 1994, 269(7): 4895-4902.
pmid: 8106462 |
| [67] |
Yang WX, Tanaka Y, Bundo M, Hirokawa N. Antioxidant signaling involving the microtubule motor KIF12 is an intracellular target of nutrition excess in beta cells. Dev Cell, 2014, 31(2): 202-214.
doi: 10.1016/j.devcel.2014.08.028 pmid: 25373778 |
| [68] |
Sampson SR, Bucris E, Horovitz-Fried M, Parnas A, Kahana S, Abitbol G, Chetboun M, Rosenzweig T, Brodie C, Frankel S. Insulin increases H2O2-induced pancreatic beta cell death. Apoptosis, 2010, 15(10): 1165-1176.
doi: 10.1007/s10495-010-0517-5 pmid: 20544287 |
| [69] |
Rharass T, Lemcke H, Lantow M, Kuznetsov SA, Weiss DG, Panáková D. Ca2+-mediated mitochondrial reactive oxygen species metabolism augments Wnt/β-catenin pathway activation to facilitate cell differentiation. J Biol Chem, 2014, 289(40): 27937-27951.
doi: 10.1074/jbc.M114.573519 pmid: 25124032 |
| [70] |
Reczek CR, Chandel NS. ROS-dependent signal transduction. Curr Opin Cell Biol, 2015, 33: 8-13.
doi: 10.1016/j.ceb.2014.09.010 pmid: 25305438 |
| [71] |
Zuo L, Zhou T, Pannell BK, Ziegler AC, Best TM. Biological and physiological role of reactive oxygen species - the good, the bad and the ugly. Acta Physiol, 2015, 214(3): 329-348.
doi: 10.1111/apha.12515 |
| [72] |
Kitamura T.The role of FOXO1 in β-cell failure and type 2 diabetes mellitus. Nat Rev Endocrinol, 2013, 9(10): 615-623.
doi: 10.1038/nrendo.2013.157 |
| [73] |
Palikaras K, Lionaki E, Tavernarakis N. Mechanisms of mitophagy in cellular homeostasis, physiology and pathology. Nat Cell Biol, 2018, 20(9): 1013-1022.
doi: 10.1038/s41556-018-0176-2 pmid: 30154567 |
| [74] |
Zeng C, Mulas F, Sui YH, Guan T, Miller N, Tan YL, Liu FF, Jin W, Carrano AC, Huising MO, Shirihai OS, Yeo GW, Sander M. Pseudotemporal ordering of single cells reveals metabolic control of postnatal β cell proliferation. Cell Metab, 2017, 25(5): 1160-1175.e1111.
doi: S1550-4131(17)30219-X pmid: 28467932 |
| [75] |
Baumel-Alterzon S, Katz LS, Brill G, Jean-Pierre C, Li YS, Tse I, Biswal S, Garcia-Ocaña A, Scott DK. Nrf 2 regulates β-cell mass by suppressing β-cell death and promoting β-cell proliferation. Diabetes, 2022, 71(5): 989-1011.
doi: 10.2337/db21-0581 pmid: 35192689 |
| [76] |
Ehses JA, Perren A, Eppler E, Ribaux P, Pospisilik JA, Maor-Cahn R, Gueripel X, Ellingsgaard H, Schneider MK, Biollaz G, Fontana A, Reinecke M, Homo-Delarche F, Donath MY. Increased number of islet-associated macrophages in type 2 diabetes. Diabetes, 2007, 56(9): 2356-2370.
pmid: 17579207 |
| [77] |
Böni-Schnetzler M, Ehses JA, Faulenbach M, Donath MY. Insulitis in type 2 diabetes. Diabetes Obes Metab, 2008, 10(Suppl 4): 201-204.
doi: 10.1111/j.1463-1326.2008.00950.x |
| [78] |
Donath MY, Shoelson SE. Type 2 diabetes as an inflammatory disease. Nat Rev Immunol, 2011, 11(2): 98-107.
doi: 10.1038/nri2925 pmid: 21233852 |
| [79] |
Cardozo AK, Ortis F, Storling J, Feng YM, Rasschaert J, Tonnesen M, Van Eylen F, Mandrup-Poulsen T, Herchuelz A, Eizirik DL. Cytokines downregulate the sarcoendoplasmic reticulum pump Ca2+ ATPase 2b and deplete endoplasmic reticulum Ca2+, leading to induction of endoplasmic reticulum stress in pancreatic beta-cells. Diabetes, 2005, 54(2): 452-461.
doi: 10.2337/diabetes.54.2.452 |
| [80] |
Choudhury S, Ghosh S, Gupta P, Mukherjee S, Chattopadhyay S. Inflammation-induced ROS generation causes pancreatic cell death through modulation of Nrf2/NF-κB and SAPK/JNK pathway. Free Radic Res, 2015, 49(11): 1371-1383.
doi: 10.3109/10715762.2015.1075016 |
| [81] |
Hansen JB, Tonnesen MF, Madsen AN, Hagedorn PH, Friberg J, Grunnet LG, Heller RS, Nielsen A, Størling J, Baeyens L, Anker-Kitai L, Qvortrup K, Bouwens L, Efrat S, Aalund M, Andrews NC, Billestrup N, Karlsen AE, Holst B, Pociot F, Mandrup-Poulsen T. Divalent metal transporter 1 regulates iron-mediated ROS and pancreatic β cell fate in response to cytokines. Cell Metab, 2012, 16(4): 449-461.
doi: 10.1016/j.cmet.2012.09.001 pmid: 23000401 |
| [82] |
Yong J, Parekh VS, Reilly SM, Nayak J, Chen ZJ, Lebeaupin C, Jang I, Zhang JW, Prakash TP, Sun H, Murray S, Guo SL, Ayala JE, Satin LS, Saltiel AR, Kaufman RJ. Chop/Ddit 3 depletion in β cells alleviates ER stress and corrects hepatic steatosis in mice. Sci Transl Med, 2021, 13(604): eaba9796.
doi: 10.1126/scitranslmed.aba9796 |
| [83] |
Han J, Backa SH, Hur J, Lin YH, Gildersleeve R, Shan JX, Yuan CL, Krokowski D, Wang SY, Hatzoglou M, Kilberg MS, Sartor MA, Kaufman RJ. ER-stress-induced transcriptional regulation increases protein synthesis leading to cell death. Nat Cell Biol, 2013, 15(5): 481-490.
doi: 10.1038/ncb2738 |
| [84] |
Lin JH, Li H, Yasumura D, Cohen HR, Zhang C, Panning B, Shokat KM, Lavail MM, Walter P. IRE 1 signaling affects cell fate during the unfolded protein response. Science, 2007, 318(5852): 944-949.
doi: 10.1126/science.1146361 pmid: 17991856 |
| [85] |
Yang Y, Cai ZX, Pan ZH, Liu F, Li DD, Ji YJ, Zhong JX, Luo HR, Hu SB, Song L, Yu SJ, Li T, Li JQ, Ma XH, Zhang WP, Zhou ZG, Liu F, Zhang JJ. Rheb 1 promotes glucose-stimulated insulin secretion in human and mouse β-cells by upregulating GLUT expression. Metabolism, 2021, 123: 154863.
doi: 10.1016/j.metabol.2021.154863 |
| [86] |
Yang WL, Chi YJ, Meng YH, Chen ZZ, Xiang R, Yan H, Yang JC. FAM3A plays crucial roles in controlling PDX1 and insulin expressions in pancreatic beta cells. FASEB J, 2020, 34(3): 3915-3931.
doi: 10.1096/fj.201902368RR pmid: 31944392 |
| [87] |
Talchai C, Xuan SH, Lin HV, Sussel L, Accili D. Pancreatic beta cell dedifferentiation as a mechanism of diabetic beta cell failure. Cell, 2012, 150(6): 1223-1234.
doi: 10.1016/j.cell.2012.07.029 |
| [88] |
Zeeshan HM, Lee GH, Kim HR, Chae HJ. Endoplasmic reticulum stress and associated ROS. Int J Mol Sci, 2016, 17(3): 327.
doi: 10.3390/ijms17030327 pmid: 26950115 |
| [89] |
Chow J, Rahman J, Achermann JC, Dattani MT, Rahman S. Mitochondrial disease and endocrine dysfunction. Nat Rev Endocrinol, 2017, 13(2): 92-104.
doi: 10.1038/nrendo.2016.151 pmid: 27716753 |
| [90] | Yoon YS, Yoon DS, Lim IK, Yoon SH, Chung HY, Rojo M, Malka F, Jou MJ, Martinou JC, Yoon G.Formation of elongated giant mitochondria in DFO-induced cellular senescence: involvement of enhanced fusion process through modulation of Fis1. J Cell Physiol, 2006, 209(2): 468-480. |
| [91] |
Schultz J, Waterstradt R, Kantowski T, Rickmann A, Reinhardt F, Sharoyko V, Mulder H, Tiedge M, Baltrusch S. Precise expression of Fis1 is important for glucose responsiveness of beta cells. J Endocrinol, 2016, 230(1): 81-91.
doi: 10.1530/JOE-16-0111 pmid: 27179109 |
| [92] |
Dandona P, Thusu K, Cook S, Snyder B, Makowski J, Armstrong D, Nicotera T. Oxidative damage to DNA in diabetes mellitus. Lancet, 1996, 347(8999): 444-445.
pmid: 8618487 |
| [93] |
Al-Aubaidy HA, Jelinek HF. Oxidative DNA damage and obesity in type 2 diabetes mellitus. Eur J Endocrinol, 2011, 164(6): 899-904.
doi: 10.1530/EJE-11-0053 pmid: 21436346 |
| [94] |
Eguchi K, Manabe I, Oishi-Tanaka Y, Ohsugi M, Kono N, Ogata F, Yagi N, Ohto U, Kimoto M, Miyake K, Tobe K, Arai H, Kadowaki T, Nagai R. Saturated fatty acid and TLR signaling link beta cell dysfunction and islet inflammation. Cell Metab, 2012, 15(4): 518-533.
doi: 10.1016/j.cmet.2012.01.023 pmid: 22465073 |
| [95] |
Ivovic A, Oprescu AI, Koulajian K, Mori Y, Eversley JA, Zhang L, Nino-Fong R, Lewis GF, Donath MY, Karin M, Wheeler MB, Ehses J, Volchuk A, Chan CB, Giacca A. IKKβ inhibition prevents fat-induced beta cell dysfunction in vitro and in vivo in rodents. Diabetologia, 2017, 60(10): 2021-2032.
doi: 10.1007/s00125-017-4345-9 pmid: 28725915 |
| [96] |
Morgan MJ, Liu ZG. Crosstalk of reactive oxygen species and NF-κB signaling. Cell Res, 2011, 21(1): 103-115.
doi: 10.1038/cr.2010.178 pmid: 21187859 |
| [97] |
Yang BY, Yang L, Wang YY, Maddison LA, Tang ZH, Haigh S, Gong YL, Zhang Y, Covington BA, Bosma KJ, Tong X, Page-McCaw P, Gannon M, Deng Q, Chen WB. Macrophages and neutrophils are necessary for ER stress-induced β cell loss. Cell Rep, 2022, 40(8): 111255.
doi: 10.1016/j.celrep.2022.111255 |
| [98] |
Salazar J, Angarita L, Morillo V, Navarro C, Martínez MS, Chacín M, Torres W, Rajotia A, Rojas M, Cano C, Añez R, Rojas J, Bermudez V. Microbiota and diabetes mellitus: role of lipid mediators. Nutrients, 2020, 12(10): 3039.
doi: 10.3390/nu12103039 |
| [99] |
Schwandner R, Dziarski R, Wesche H, Rothe M, Kirschning CJ.Peptidoglycan- and lipoteichoic acid- induced cell activation is mediated by toll-like receptor 2. J Biol Chem, 1999, 274(25): 17406-17409.
doi: 10.1074/jbc.274.25.17406 pmid: 10364168 |
| [100] |
Gao H, Luo ZL, Ji YD, Tang KC, Jin ZM, Ly C, Sears DD, Mahata S, Ying W. Accumulation of microbial DNAs promotes to islet inflammation and β cell abnormalities in obesity in mice. Nat Commun, 2022, 13(1): 565.
doi: 10.1038/s41467-022-28239-2 pmid: 35091566 |
| [101] |
Cinti F, Bouchi R, Kim-Muller JY, Ohmura Y, Sandoval PR, Masini M, Marselli L, Suleiman M, Ratner LE, Marchetti P, Accili D. Evidence of beta-cell dedifferentiation in human type 2 diabetes. J Clin Endocrinol Metab, 2016, 101(3): 1044-1054.
doi: 10.1210/jc.2015-2860 |
| [102] |
Spijker HS, Ravelli RBG, Mommaas-Kienhuis AM, van Apeldoorn AA, Engelse MA, Zaldumbide A, Bonner- Weir S, Rabelink TJ, Hoeben RC, Clevers H, Mummery CL, Carlotti F, de Koning EJP. Conversion of mature human beta-cells into glucagon-producing alpha-cells. Diabetes, 2013, 62(7): 2471-2480.
doi: 10.2337/db12-1001 pmid: 23569174 |
| [103] |
Collombat P, Mansouri A, Hecksher-Sorensen J, Serup P, Krull J, Gradwohl G, Gruss P. Opposing actions of Arx and Pax4 in endocrine pancreas development. Genes Dev, 2003, 17(20): 2591-2603.
doi: 10.1101/gad.269003 |
| [104] |
Sosa-Pineda B, Chowdhury K, Torres M, Oliver G, Gruss P. The Pax4 gene is essential for differentiation of insulin-producing beta cells in the mammalian pancreas. Nature, 1997, 386(6623): 399-402.
doi: 10.1038/386399a0 |
| [105] |
Ilegems E, Bryzgalova G, Correia J, Yesildag B, Berra E, Ruas JL, Pereira TS, Berggren PO. HIF-1α inhibitor PX- 478 preserves pancreatic β cell function in diabetes. Sci Transl Med, 2022, 14(638): eaba9112.
doi: 10.1126/scitranslmed.aba9112 |
| [106] |
Preissl S, Gaulton KJ, Ren B. Characterizing cis- regulatory elements using single-cell epigenomics. Nat Rev Genet, 2022, doi: 10.1038/s41576-022-00509-1.
doi: 10.1038/s41576-022-00509-1 |
| [1] | Yang Yang, Mingxing Chu, Qiuyue Liu. The mechanism of circadian clock and its influence on animal circannual rhythm [J]. Hereditas(Beijing), 2023, 45(5): 409-424. |
| [2] | Shanshan Gao, Jinliang Li, Jiani Yang, Tong Zhou, Rui Liu, Xiaoping Wang, Li Yu. Progresses on adaptive evolution of gliding and flying ability in mammals [J]. Hereditas(Beijing), 2022, 44(1): 46-58. |
| [3] | Zhiyang Zeng, Jiawei Lu, Xiya Cao, Xinyue Wang, Dali Li. A method for constructing GLP-1 overexpression intestinal organoids [J]. Hereditas(Beijing), 2021, 43(7): 694-703. |
| [4] | Lan Cao, Zhiqiang Li, Yongyong Shi, Yun Liu. Telomere length and type 2 diabetes: Mendelian randomization study and polygenic risk score analysis [J]. Hereditas(Beijing), 2020, 42(9): 882-888. |
| [5] | Lian Ren, Xiushan Wu, Yongqing Li. The mechanism underlying histone deacetylases regulating cardiac hypertrophy [J]. Hereditas(Beijing), 2020, 42(6): 536-547. |
| [6] | Yuzhuo Wang, Yiming Zhang, Xiaolian Dong, Xuecai Wang, Jianfu Zhu, Na Wang, Feng Jiang, Yue Chen, Qingwu Jiang, Chaowei Fu. Modification effects of T2DM-susceptible SNPs on the reduction of blood glucose in response to lifestyle interventions [J]. Hereditas(Beijing), 2020, 42(5): 483-492. |
| [7] | Xianci Xue,Li Yu. Advances on polyphenism in insects [J]. Hereditas(Beijing), 2017, 39(9): 798-809. |
| [8] | Xian Gong, Chao Zhang, Aisa Yiliyasi, Ying Shi, Xuewei Yang, Aosiman Nuersimanguli, Yaqun Guan, Shuhua Xu. A comparative analysis of genetic diversity of candidate genes associated with type 2 diabetes in worldwide populations [J]. Hereditas(Beijing), 2016, 38(6): 543-559. |
| [9] | Ri Wu,Chao Ma,Xiaodan Li,Huikun Duan,Yanli Ji,Yu Wang,Pingzhe Jiang,Haisong Wang,Peipei Tu,Miao Li,Ganggang Ni,Baicheng Ma,Minggang Li. Construction of yeast strains expressing long-acting glucagon-like peptide-1 (GLP-1) and their therapeutic effects on type 2 diabetes mellitus mouse model [J]. HEREDITAS(Beijing), 2015, 37(2): 183-191. |
| [10] | Xiaohua Yang, Huafeng Zhang, Jianghua Lai. Alcohol dependence mediated by monoamine neurotransmitters in the central nervous system [J]. HEREDITAS, 2014, 36(1): 11-20. |
| [11] | XU Chen-Lu, SUN Xiao-Mei, ZHANG Shou-Gong. Mechanism on differential gene expression and heterosis formation [J]. HEREDITAS, 2013, 35(6): 714-726. |
| [12] | TANG Lin-Lin LIU Qiong BU Shi-Zhong XU Lei-Ting WANG Qin-Wen MAI Yi-Feng DUAN Shi-Wei. The effect of environmental factors and DNA methylation on type 2 diabetes mellitus [J]. HEREDITAS, 2013, 35(10): 1143-1152. |
| [13] | LI Ze-Qin LI Jing-Xiao ZHANG Gen-Fa. Expression regulation of plant ascorbate peroxidase and its tolerance to abiotic stresses [J]. HEREDITAS, 2013, 35(1): 45-54. |
| [14] | PU Lian-Mei, NAN Nan, YANG Ze, JIN Ze-Ning. Association between SUMO4 polymorphisms and type 2 diabetes mellitus [J]. HEREDITAS, 2012, 34(3): 315-325. |
| [15] | TANG Xiao-Li, DENG Li-Bin, LI Gui-Lin, LIU Shuang-Mei, LIN Jia-Ri, XIE Jin-Yan, LIU Jun, KONG Fan-Jun, LIANG Shang-Dong. Analysis of gene expression profile of peripheral ganglia in early stage type Ⅱ diabetic rats [J]. HEREDITAS, 2012, 34(2): 198-207. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||