Hereditas(Beijing) ›› 2022, Vol. 44 ›› Issue (11): 1079-1086.doi: 10.16288/j.yczz.22-210
• Genetic Resource • Previous Articles
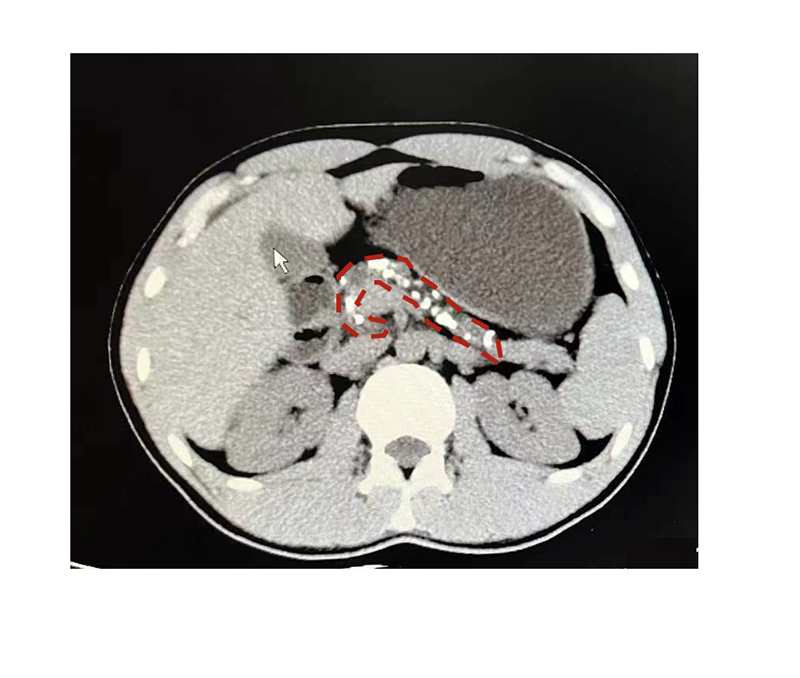
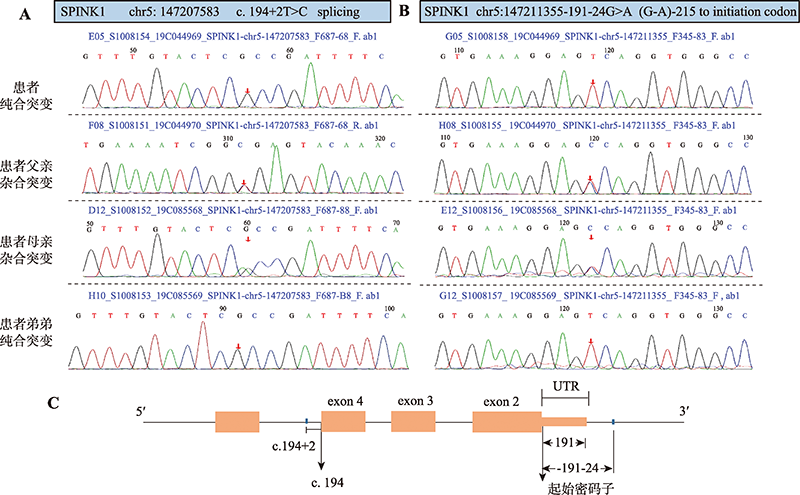
Diagnosis, treatment and genetic analysis of a case with fibrocalculous pancreatic diabetes
Min Shen1( ), Yong Gu1, Changjiang Ying2, Mei Zhang1, Tao Yang1, Yang Chen1(
), Yong Gu1, Changjiang Ying2, Mei Zhang1, Tao Yang1, Yang Chen1( )
)
- 1. Department of Endocrinology, First Affiliated Hospital of Nanjing Medical University, Nanjing 210029, China
2. Department of Endocrinology, The Affiliated Hospital of Xuzhou Medical University, Xuzhou 221000, China
-
Received:2022-06-21Revised:2022-09-01Online:2022-11-20Published:2022-09-07 -
Contact:Chen Yang E-mail:drshenmin@163.com;drchenyang@njmu.edu.cn -
Supported by:the National Natural Science Foundation of China(81900708);Postgraduate Research & Practice Innovation Program of Jiangsu Province(JX10213850);Sinocare Diabetes Foundation(2021SD02)
Cite this article
Min Shen, Yong Gu, Changjiang Ying, Mei Zhang, Tao Yang, Yang Chen. Diagnosis, treatment and genetic analysis of a case with fibrocalculous pancreatic diabetes[J]. Hereditas(Beijing), 2022, 44(11): 1079-1086.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
Table 1
Clinical information of the family"
| 项目 | 患者父亲 | 患者母亲 | 患者弟弟 |
|---|---|---|---|
| 年龄 | 50 | 52 | 16 |
| 体重指数(kg/m2) | 26.2 | 19.9 | 29.39 |
| 空腹血糖(mmol/L) | 5.29 | 5.11 | 4.82 |
| 餐后1 h血糖(mmol/L) | - | 9.26 | 8.26 |
| 餐后2 h血糖(mmol/L) | 8.78 | 9.2 | 6.53 |
| 空腹胰岛素(pmol/L) | 70.3 | 36.8 | 72 |
| 餐后1 h胰岛素(pmol/L) | - | 403.4 | 404.3 |
| 餐后2 h胰岛素(pmol/L) | 834.6 | 312.8 | 678.5 |
| 空腹C肽(ng/mL) | 2.09 | 1.8 | 2.04 |
| 餐后1 h C肽(ng/mL) | - | 9.47 | 8.37 |
| 餐后2 h C肽(ng/mL) | 14.68 | 11.39 | 11.21 |
| 持续性腹痛 | 无 | 无 | 无 |
| 胰腺影像学检查 | - | 胰腺未见异常 | 胰腺未见异常 |
Table 2
Comparison of clinical characteristics of FCPD at home and abroad"
| 国内报道 | 国外报道 | 本例患者 | |
|---|---|---|---|
| 发病率 | <0.001% | 0.019%~1.6% | - |
| 地区分布 | 散在分布,亚热带和北温带为主 | 热带为主 | 中国北温带 |
| 年龄 | 16~67 | 10~30岁多见 | 25 |
| 性别(男%) | 64% | 43%~70% | 男 |
| BMI (kg/m2) | 多消瘦 | 多消瘦 | 17.17 |
| 木薯食用史 | 20% | 常见 | 否 |
| 降糖治疗 | 胰岛素治疗为主 | 胰岛素治疗为主 | 口服药 |
| 误诊 | >20% | >85% | 否 |
| 脂肪泻(%) | <30% | 24% | 否 |
| 慢性腹痛(%) | 50% | 33% | 是 |
| 胰岛自身抗体 | 1例GAD阳性 | GAD阳性:7.0% ICA阳性:6.3% | IAA阳性后转阴 |
| 基因 | WFS1基因2号外显子杂合突变: c.139C>T | HLA-DQ9 (A*0201-B*0303),DQB1; SPINK1基因最常见 | HLA-A*2402;3201, DRB1*0701;1301,SPINK1基因纯合突变:c.194+2T>C与-191-24G>A |
| [1] |
Bhat JA, Bhat MH, Misgar RA, Bashir MI, Wani AI, Masoodi SR, Ashraf H, Sood M. The clinical spectrum of fibrocalculous pancreatic diabetes in kashmir valley and comparative study of the clinical profile of fibrocalculous pancreatic diabetes and type 2 diabetes mellitus. Indian J Endocrinol Metab, 2019, 23(5): 580-584.
doi: 10.4103/ijem.IJEM_297_19 pmid: 31803601 |
| [2] | Feng SS, Wang S. Diagnosis and treatment of a case of fibrocalculous pancreatic diabetes. Shangdong Med J, 2021, 61(21): 84-87. |
| 冯姗姗, 王肃. 1例胰腺纤维钙化性糖尿病的诊断及治疗. 山东医药, 2021, 61(21): 84-87. | |
| [3] | Chi HY, Wang AH, Liu YJ, Zhou YP. Fibrocalculous pancreatic diabetes: one case report and literature review. Chin J Endocrinol Metab, 2014, (8): 701-704. |
| 迟海燕, 王爱红, 刘彦君, 周玉萍. 胰腺纤维钙化性糖尿病一例并文献复习. 中华内分泌代谢杂志, 2014, (8): 701-704. | |
| [4] | Yang SL, Chen M, Li N, Xu L, Luo YL, Zhang MN, Bu L, Lin ZW, Li H, Qu S. Fibrocalculous pancreatic diabetes: one case report and literature review. Int J Endocrinol Metab, 2017, 37 (5): 355-357. |
| 杨绍玲, 陈铭, 李楠, 徐璐, 罗伊丽, 张曼娜, 卜乐, 林紫薇, 李鸿, 曲伸. 胰腺纤维钙化性糖尿病1例并文献复习. 国际内分泌代谢杂志, 2017, 37(5): 355-357. | |
| [5] | Pan JX, Jiang F, Sun MY, Lin F. Fibrocalculous pancreatic diabetes: one case report and literature review. Chin J Diabetes, 2017, 25(6): 563-564. |
| 潘金兴, 姜锋, 孙铭遥, 林帆. 胰腺纤维钙化性糖尿病一例报告及文献复习. 中国糖尿病杂志, 2017, 25(6): 563-564. | |
| [6] | Cha XY, Wei CS, Lai PB. Analysis of clinical characteristics of 16 cases with fibrocalculous pancreatic diabetes and literature review. Fujian Med J, 2020, 42(4): 14-17. |
| 查小云, 魏长顺, 赖鹏斌. 胰腺纤维钙化性糖尿病16例临床特点分析并文献复习. 福建医药杂志, 2020, 42(4): 14-17. | |
| [7] | Liu XM, Ouyang LL, Xian Su, Wang WQ. Two cases of calcareous pancreatitis of family resulted diabetes mellitus. J Clin Intern Med, 2001, 18(3): 236. |
| 刘晓梅, 欧阳玲莉, 冼苏, 王文清. 家族性钙化性胰腺炎致糖尿病二例. 临床内科杂志, 2001, 18(3): 236. | |
| [8] | Chen YL, Chen GF, Liu C. Fibrocalculous pancreatic diabetes: a case report and literature review. Chin J Endocrinol Metab, 2021, 37(2): 165-167. |
| 陈彦乐, 陈国芳, 刘超. 胰腺纤维钙化性糖尿病一例并文献复习. 中华内分泌代谢杂志, 2021, 37(2): 165-167. | |
| [9] | Li YR, Yu ZQ, Pan HL, Hong Y. Clinical and laboratory study on tropical pancreatic diabetes. J Guangxi Med Univ, 1998, 15(2): 11-13. |
| 黎英荣, 于志清, 潘海林, 洪英. 热带胰腺性糖尿病的临床特点及实验室研究. 广西医科大学学报, 1998, 15(2): 11-13. | |
| [10] | Wang J, Tian HM, Liang JZ. Pancreaticolithiasis and fibrocalcific diabetes mellitus. West China Med J, 1995, 10(4): 403-404. |
| 王静, 田浩明, 梁荩忠. 胰石症与胰腺纤维钙化性糖尿病. 华西医学, 1995, 10(4): 403-404. | |
| [11] | Jia Q, Zhang Y, Ma KN. Fibrocalcuous pancreatic diabetes:8 cases report. J Liaoning Pract Diabetes, 2001, 9(3): 39-40. |
| 贾奇, 张音, 马克宁. 胰腺纤维化结石性糖尿病(附8例报告). 辽宁实用糖尿病杂志, 2001, 9(3): 39-40. | |
| [12] | Li YJ, Su HY. Fibrocalculous pancreatic diabetes: one case report. Chin J Diabetes, 2014, 22(12): 1136-1137. |
| 李勇杰, 苏宏业. 胰腺纤维钙化性糖尿病一例报告. 中国糖尿病杂志, 2014, 22(12): 1136-1137. | |
| [13] | Shi Y. Pancreatic fibrotic calculous diabetes mellitus: a case report and literature review. J Hepatobiliary Surg, 2003, 11(6): 449-451. |
| 施勇. 胰腺纤维化结石性糖尿病(附1例报告并文献复习). 肝胆外科杂志, 2003, 11(6): 449-451 | |
| [14] | Chen JZ, Li J, Zhu KX. Fibrocalculous pancreatic diabetes misdiagnosed as type 1 diabetes for years: a case report and literature review. Acad J Chin PLA Med Sch, 2020, 41(7): 752-754. |
| 陈炯镇, 李佳, 朱凯旋. 胰腺纤维钙化性糖尿病长期误诊为1型糖尿病1例报告并文献复习. 解放军医学院学报, 2020, 41(7): 752-754. | |
| [15] | Wang JW, Yu BJ, Chen P. Chen YT. Fibrocalcuous pancreatic diabetes: a case report. Chin J Rural Med Pharm, 2020, 27(16): 38-39. |
| 王金委, 俞碧君, 陈平, 陈盈婷. 胰腺纤维钙化性糖尿病1例. 中国乡村医药, 2020, 27(16): 38-39. | |
| [16] | Li WG, Deng YH, Mai KY. Fibrocalcuous pancreatic diabetes complicated with osteoporosis: a case report. Guangdong Med J, 2020, 21(10): 844. |
| 李万根, 邓煜辉, 麦坤仪. 胰腺纤维钙化性糖尿病并骨质疏松症1例. 广东医学, 2020, 21(10): 844. | |
| [17] | Liu B, Yu RP, Luo JH, Long BD. Fibrocalcuous pancreatic diabetes misdiagnosed as type 1 diabetes. Clin Misdiagn Misther, 2011, 24(10): 70-71. |
| 刘波, 于瑞萍, 罗建华, 龙本丹. 胰腺纤维钙化性糖尿病误诊为1型糖尿病. 临床误诊误治, 2011, 24(10): 70-71. | |
| [18] | Wang YQ, Wu FX, Liang QF, Zhao YD, Wu JP. Fibrocalcuous pancreatic diabetes: a case report. Zhejiang J Integr Med, 2021, 31(2): 147-149. |
| 王云卿, 吴飞翔, 梁秋芳, 赵延栋, 吴君平. 胰腺纤维钙化性糖尿病一例报道. 浙江中西医结合杂志, 2021, 31(2): 147-149. | |
| [19] | Deng YY, Zhang JL, Qiu L. Pancreatic fibrotic calculous diabetes mellitus: a case report and literature review. Clin Focus, 2015, 30(12): 1433-1434. |
| 邓英英, 张晶露, 邱琳. 胰腺纤维钙化性糖尿病2例并文献复习. 临床荟萃, 2015, 30(12): 1433-1434. | |
| [20] | Ye SZ, Qian GX. Fibrocalculous pancreatic diabetes:10 cases report. Chin J Endocrinol Metab, 1991, 7(4): 198-200. |
| 叶绍珍, 钱光相. 胰纤维化结石性糖尿病(附10例报告). 中华内分泌代谢杂志, 1991, 7(4): 198-200. | |
| [21] | Pei Y, Pang P, Wang HZ, Han XF, Wang XL, Du J, Yang GQ, Lv ZH, Mu YM, Lu JM, Dou JT. Three cases of fibrocalculous pancreatic diabetes and review of literatures. Chin J Diabetes Mellitus, 2012, 4(12): 713-717. |
| 裴育, 庞萍, 王海珍, 韩晓菲, 王先令, 杜锦, 杨国庆, 吕朝晖, 母义明, 陆菊明, 窦京涛. 胰腺纤维钙化性糖尿病三例报告及文献复习. 中华糖尿病杂志, 2012, 4(12): 713-717. | |
| [22] | Papita R, Nazir A, Anbalagan VP, Anjana RM, Pitchumoni C, Chari S, Mohan V. Secular trends of fibrocalculous pancreatic diabetes and diabetes secondary to alcoholic chronic pancreatitis at a tertiary care diabetes centre in South India. JOP, 2012, 13(2): 205-209. |
| [23] |
Kolly A, Shivaprasad C, Pulikkal AA, Atluri S, Sarathi V, Dwarakanath CS. High prevalence of serine protease inhibitor Kazal type 1 gene variations detected by whole gene sequencing in patients with fibrocalculous Pancreatic Diabetes. Indian J Endocrinol Metab, 2017, 21(4): 510-514.
doi: 10.4103/ijem.IJEM_116_17 pmid: 28670531 |
| [24] |
Chowdhury ZM, McDermott MF, Davey S, Hassan Z, Sinnott PJ, Hemmatpour SK, Sherwin S, Ali L, Aganna E, Allotey RA, North BV, Cassell PG, Azad Khan AK, Hitman GA. Genetic susceptibility to fibrocalculous pancreatic diabetes in Bangladeshi subjects: a family study. Genes Immun, 2002, 3(1): 5-8.
pmid: 11857053 |
| [25] |
Mohan V, Nagalotimath SJ, Yajnik CS, Tripathy BB. Fibrocalculous pancreatic diabetes. Diabetes Metab Rev, 1998, 14(2): 153-170.
pmid: 9679668 |
| [26] |
Kibirige D, Kibudde S, Mutebi E. Fibrocalculous pancreatic diabetes in a young Ugandan patient, a rare form of secondary diabetes. BMC Res Notes, 2012, 5(1): 622-624.
doi: 10.1186/1756-0500-5-622 |
| [27] |
Li MH, Wang SH, Xu KF, Chen Y, Fu Q, Gu Y, Shi Y, Zhang M, Sun M, Chen H, Han XQ, Li YX, Tang ZK, Cai LJ, Li ZQ, Shi YY, Yang T, Polychronakos C. High prevalence of a monogenic cause in Han Chinese diagnosed with type 1 diabetes, partly driven by nonsyndromic recessive WFS1 mutations. Diabetes, 2020, 69(1): 121-126.
doi: 10.2337/db19-0510 |
| [28] |
Ghosh I, Mukhopadhyay P, Das K, Anne M B, Ali Mondal S, Basu M, Nargis T, Pandit K, Chakrabarti P, Ghosh S. Incretins in fibrocalculous pancreatic diabetes: a unique subtype of pancreatogenic diabetes. J Diabetes, 2021, 13(6): 506-511.
doi: 10.1111/1753-0407.13139 pmid: 33247879 |
| [29] |
Barman KK, Premalatha G, Mohan V. Tropical chronic pancreatitis. Postgrad Med J, 2003, 79(937): 606-615.
pmid: 14654569 |
| [30] |
Chari ST, Mohan V, Pitchumoni CS, Viswanathan M, Madanagopalan N, Lowenfels AB. Risk of pancreatic carcinoma in tropical calcifying pancreatitis: an epidemiologic study. Pancreas, 1994, 9(1): 62-66.
doi: 10.1097/00006676-199401000-00009 |
| [1] | Huijie Yang, De Li, Huiling Bai, Ming Zhang, Jun Huang, Xiaoqing Yuan. Diagnosis, treatment and genetic analysis of a case of Alstrom syndrome caused by compoud heterozygous mutation of ALMS1 [J]. Hereditas(Beijing), 2022, 44(12): 1148-1157. |
| [2] | Jingya Ye, Aijie Huang, Zhenzhen Fu, Yingyun Gong, Hongyuan Yang, Hongwen Zhou. A study of congenital generalized lipodystrophy (CGL) caused by BSCL2 gene mutation [J]. Hereditas(Beijing), 2022, 44(10): 926-936. |
| [3] | Chengan Lv, Ruoran Wang, Zhuo-Xian Meng. Molecular mechanism of islet β-cell functional alternations during type 2 diabetes [J]. Hereditas(Beijing), 2022, 44(10): 840-852. |
| [4] | Liwen Zhang, Meihua Ruan, Jialan Liu, Caihong He, Jianrong Yu. Progress on research and development in diabetes mellitus [J]. Hereditas(Beijing), 2022, 44(10): 824-839. |
| [5] | Zhiyang Zeng, Jiawei Lu, Xiya Cao, Xinyue Wang, Dali Li. A method for constructing GLP-1 overexpression intestinal organoids [J]. Hereditas(Beijing), 2021, 43(7): 694-703. |
| [6] | Lan Cao, Zhiqiang Li, Yongyong Shi, Yun Liu. Telomere length and type 2 diabetes: Mendelian randomization study and polygenic risk score analysis [J]. Hereditas(Beijing), 2020, 42(9): 882-888. |
| [7] | Yuzhuo Wang, Yiming Zhang, Xiaolian Dong, Xuecai Wang, Jianfu Zhu, Na Wang, Feng Jiang, Yue Chen, Qingwu Jiang, Chaowei Fu. Modification effects of T2DM-susceptible SNPs on the reduction of blood glucose in response to lifestyle interventions [J]. Hereditas(Beijing), 2020, 42(5): 483-492. |
| [8] | Xin Huang,Yongqiang Chen,Guoliang Xu,Shuhong Peng. DNA methylation in adipose tissue and the development of diabetes and obesity [J]. Hereditas(Beijing), 2019, 41(2): 98-110. |
| [9] | Xian Gong, Chao Zhang, Aisa Yiliyasi, Ying Shi, Xuewei Yang, Aosiman Nuersimanguli, Yaqun Guan, Shuhua Xu. A comparative analysis of genetic diversity of candidate genes associated with type 2 diabetes in worldwide populations [J]. Hereditas(Beijing), 2016, 38(6): 543-559. |
| [10] | Ri Wu,Chao Ma,Xiaodan Li,Huikun Duan,Yanli Ji,Yu Wang,Pingzhe Jiang,Haisong Wang,Peipei Tu,Miao Li,Ganggang Ni,Baicheng Ma,Minggang Li. Construction of yeast strains expressing long-acting glucagon-like peptide-1 (GLP-1) and their therapeutic effects on type 2 diabetes mellitus mouse model [J]. HEREDITAS(Beijing), 2015, 37(2): 183-191. |
| [11] | Mingjun Cao, Huansheng Dong, Qingjie Pan, Hongjun Wang, Xiao Dong. Progress in early pancreas development and reprogramming of terminally differentiated cells into β cells [J]. HEREDITAS(Beijing), 2014, 36(6): 511-518. |
| [12] | TANG Lin-Lin LIU Qiong BU Shi-Zhong XU Lei-Ting WANG Qin-Wen MAI Yi-Feng DUAN Shi-Wei. The effect of environmental factors and DNA methylation on type 2 diabetes mellitus [J]. HEREDITAS, 2013, 35(10): 1143-1152. |
| [13] | PU Lian-Mei, NAN Nan, YANG Ze, JIN Ze-Ning. Association between SUMO4 polymorphisms and type 2 diabetes mellitus [J]. HEREDITAS, 2012, 34(3): 315-325. |
| [14] | TANG Xiao-Li, DENG Li-Bin, LI Gui-Lin, LIU Shuang-Mei, LIN Jia-Ri, XIE Jin-Yan, LIU Jun, KONG Fan-Jun, LIANG Shang-Dong. Analysis of gene expression profile of peripheral ganglia in early stage type Ⅱ diabetic rats [J]. HEREDITAS, 2012, 34(2): 198-207. |
| [15] | WANG Min, BANG Chan, JUE E-Chi, HUANG Jing-Yang. Association and meta-analysis of ENPP1 K121Q with type 2 diabetes in Han Chinese [J]. HEREDITAS, 2010, 32(8): 808-816. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||