Hereditas(Beijing) ›› 2021, Vol. 43 ›› Issue (1): 30-39.doi: 10.16288/j.yczz.20-315
• Review • Previous Articles Next Articles
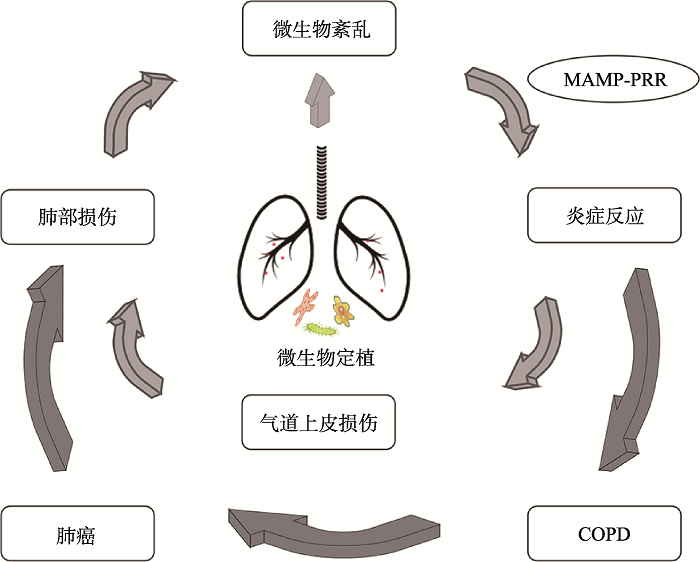
Lung microbiome mediates the progression from chronic obstructive pulmonary disease to lung cancer through inflammation
Yajie Wang, Shuangshuang Wu, Jiang Chu( ), Xiangyang Kong(
), Xiangyang Kong( )
)
- Genetics and Pharmacogenomics Laboratory, Medical School, Kunming University of Science and Technology, Kunming 650500, China
-
Received:2020-11-24Revised:2020-12-28Online:2021-01-20Published:2021-01-12 -
Contact:Chu Jiang,Kong Xiangyang E-mail:chujiang2015@126.com;kxy2772@yahoo.com -
Supported by:Supported by Provincial Training Program of Kunming University of Science and Technology No(KKSY201660006)
Cite this article
Yajie Wang, Shuangshuang Wu, Jiang Chu, Xiangyang Kong. Lung microbiome mediates the progression from chronic obstructive pulmonary disease to lung cancer through inflammation[J]. Hereditas(Beijing), 2021, 43(1): 30-39.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
| [1] | Liu YX, Qin Y, Guo XX, Bai Y . Methods and applications for microbiome data analysis. Hereditas(Beijing), 2019,41(9):845-862. |
| 刘永鑫, 秦媛, 郭晓璇, 白洋 . 微生物组数据分析方法与应用. 遗传, 2019,41(9):845-862. | |
| [2] |
Kim HJ, Kim YS, Kim KH, Choi JP, Kim YK, Yun SM, Sharma L, Cruz CSD, Lee JS, Oh YM, Lee SD, Lee SW . The microbiome of the lung and its extracellular vesicles in nonsmokers, healthy smokers and COPD patients. Exp Mol Med, 2017,49(4):e316.
doi: 10.1038/emm.2017.7 pmid: 28408748 |
| [3] |
Parris BA, O’Farrell HE, Fong KM, Yang IA. Chronic obstructive pulmonary disease (COPD) and lung cancer: Common pathways for pathogenesis. J Thorac Dis, 2019,11(Suppl.17):S2155-S2172.
doi: 10.21037/jtd.2019.10.54 pmid: 31737343 |
| [4] |
Mao QX, Jiang F, Yin R, Wang J, Xia WJ, Dong GC, Ma WD, Yang Y, Xu L, Hu JZ . Interplay between the lung microbiome and lung cancer. Cancer Lett, 2018,415:40-48.
doi: 10.1016/j.canlet.2017.11.036 pmid: 29197615 |
| [5] |
Mendez R, Banerjee S, Bhattacharya SK, Banerjee S . Lung inflammation and disease: A perspective on microbial homeostasis and metabolism. IUBMB Life, 2019,71(2):152-165.
doi: 10.1002/iub.1969 pmid: 30466159 |
| [6] | Shen YC, Chen L, Wen FQ . Interpretation of 2019 global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease. Natl Med J China, 2018,98(48):3913-3916. |
| 申永春, 陈磊, 文福强 . 2019年慢性阻塞性肺疾病全球创议更新要点. 中华医学杂志, 2018,98(48):3913-3916. | |
| [7] |
Quaderi SA, Hurst JR . The unmet global burden of COPD. Glob Health Epidemiol Genom, 2018,3:e4
doi: 10.1017/gheg.2018.1 pmid: 29868229 |
| [8] |
Fang TT, Wang MN, Xiao HY, Wei XW . Mitochondrial dysfunction and chronic lung disease. Cell Biol Toxicol, 2019,35(6):493-502.
doi: 10.1007/s10565-019-09473-9 pmid: 31119467 |
| [9] | Qian GQ . Advances in genome-wide association study of chronic obstructive pulmonary disease. Hereditas(Beijing), 2020,42(9):832-846. |
| 钱国清 . 慢性阻塞性肺疾病全基因组关联研究进展. 遗传, 2020,42(9):832-846. | |
| [10] |
Siegel RL, Miller KD, Jemal A . Cancer statistics, 2017. CA Cancer J Clin, 2017,67(1):7-30.
doi: 10.3322/caac.21387 pmid: 28055103 |
| [11] |
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A . Global cancer statistics, 2012. CA Cancer J Clin, 2015,65(2):87-108.
doi: 10.3322/caac.21262 pmid: 25651787 |
| [12] |
Houghton AM . Mechanistic links between COPD and lung cancer. Nat Rev Cancer, 2013,13(4):233-45.
doi: 10.1038/nrc3477 pmid: 23467302 |
| [13] |
Caramori G, Ruggeri P, Mumby S, Ieni A, Lo Bello F, Chimankar V, Donovan C, Andò F, Nucera F, Coppolino I, Tuccari G, Hansbro PM, Adcock IM . Molecular links between COPD and lung cancer: new targets for drug discovery? Expert Opin Ther Targets, 2019,23(6):539-553.
doi: 10.1080/14728222.2019.1615884 pmid: 31079559 |
| [14] |
Chalela R, Gea J, Barreiro E . Immune phenotypes in lung cancer patients with COPD: Potential implications for immunotherapy. J Thorac Dis, 2018,10(Suppl.18):S2186-S2189.
doi: 10.21037/jtd.2018.06.143 pmid: 30123556 |
| [15] |
Jungnickel C, Wonnenberg B, Karabiber O, Wolf A, Voss M, Wolf L, Honecker A, Kamyschnikow A, Herr C, Bals R, Beisswenger C . Cigarette smoke-induced disruption of pulmonary barrier and bacterial translocation drive tumor-associated inflammation and growth. Am J Physiol Lung Cell Mol Physiol, 2015,309(6):L605-L613.
doi: 10.1152/ajplung.00116.2015 pmid: 26209273 |
| [16] |
Dickson RP, Erb-Downward JR, Martinez FJ, Huffnagle GB . The microbiome and the respiratory tract. Annu Rev Physiol, 2016,78:481-504.
doi: 10.1146/annurev-physiol-021115-105238 pmid: 26527186 |
| [17] |
Sze MA, Dimitriu PA, Suzuki M, McDonough JE, Campbell JD, Brothers JF, Erb-Downward JR, Huffnagle GB, Hayashi S, Elliott WM, Cooper J, Sin DD, Lenburg ME, Spira A, Mohn WW, Hogg JC. Host response to the lung microbiome in chronic obstructive pulmonary disease. Am J Respir Crit Care Med, 2015,192(4):438-445.
doi: 10.1164/rccm.201502-0223OC pmid: 25945594 |
| [18] |
Budden KF, Shukla SD, Rehman SF, Bowerman KL, Keely S, Hugenholtz P, Armstrong-James DPH, Adcock IM, Chotirmall SH, Chung KF, Hansbro PM . Functional effects of the microbiota in chronic respiratory disease. Lancet Respir Med, 2019,7(10):907-920.
doi: 10.1016/S2213-2600(18)30510-1 pmid: 30975495 |
| [19] |
Mitchell AB, Glanville AR . The human respiratory microbiome: implications and impact. Semin Respir Crit Care Med, 2018,39(2):199-212.
doi: 10.1055/s-0037-1617441 pmid: 29579771 |
| [20] |
Wu BG, Segal LN . Lung microbiota and its impact on the mucosal immune phenotype. Microbiol Spectr, 2017,5(3).
doi: 10.1128/microbiolspec.FUNK-0030-2016 pmid: 28597810 |
| [21] | Moffatt MF, Cookson WO . The lung microbiome in health and disease. Clin Med (Lond), 2017,17(6):525-529. |
| [22] |
Sze MA, Dimitriu PA, Hayashi S, Elliott WM, McDonough JE, Gosselink JV, Cooper J, Sin DD, Mohn WW, Hogg JC . The lung tissue microbiome in chronic obstructive pulmonary disease. Am J Respir Crit Care Med, 2012,185(10):1073-1080.
doi: 10.1164/rccm.201111-2075OC pmid: 22427533 |
| [23] |
Faner R, Sibila O, Agustí A, Bernasconi E, Chalmers JD, Huffnagle GB, Manichanh C, Molyneaux PL, Paredes R, Brocal VP, Ponomarenko J, Sethi S, Dorca J, Monsó E . The microbiome in respiratory medicine: Current challenges and future perspectives. Eur Respir J, 2017,49(4):1602086.
doi: 10.1183/13993003.02086-2016 pmid: 28404649 |
| [24] |
Dima E, Kyriakoudi A, Kaponi M, Vasileiadis I, Stamou P, Koutsoukou A, Koulouris NG, Rovina N . The lung microbiome dynamics between stability and exacerbation in chronic obstructive pulmonary disease (COPD): Current perspectives. Respir Med, 2019,157:1-6.
doi: 10.1016/j.rmed.2019.08.012 pmid: 31450162 |
| [25] |
Welp AL, Bomberger JM . Bacterial community interactions during chronic respiratory disease. Front Cell Infect Microbiol, 2020,10:213.
doi: 10.3389/fcimb.2020.00213 pmid: 32477966 |
| [26] |
Garcia-Nuñez M, Millares L, Pomares X, Ferrari R, Pérez-Brocal V, Gallego M, Espasa M, Moya A, Monsó E . Severity-related changes of bronchial microbiome in chronic obstructive pulmonary disease. J Clin Microbiol, 2014,52(12):4217-4223.
doi: 10.1128/JCM.01967-14 |
| [27] |
Pragman AA, Lyu T, Baller JA, Gould TJ, Kelly RF, Reilly CS, Isaacson RE, Wendt CH . The lung tissue microbiota of mild and moderate chronic obstructive pulmonary disease. Microbiome, 2018,6(1):7.
doi: 10.1186/s40168-017-0381-4 pmid: 29316977 |
| [28] |
Monsó E . Microbiome in chronic obstructive pulmonary disease. Ann Transl Med, 2017,5(12):251.
doi: 10.21037/atm.2017.04.20 pmid: 28706919 |
| [29] |
Galiana A, Aguirre E, Rodriguez JC, Mira A, Santibanẽz M, Candela I, Llavero J, Garcinunõ P, Loṕez F, Ruiz M, Garcia-Pachon E, Royo G. Sputum microbiota in moderate versus severe patients with COPD. Eur Respir J, 2014,43(6):1787-1790.
doi: 10.1183/09031936.00191513 pmid: 24311775 |
| [30] |
Millares L, Pérez-Brocal V, Ferrari R, Gallego M, Pomares X, García-Núñez M, Montón C, Capilla S, Monsó E, Moya A . Functional metagenomics of the bronchial microbiome in COPD. PLoS One, 2015,10(12):e0144448.
doi: 10.1371/journal.pone.0144448 pmid: 26632844 |
| [31] |
Mur LA, Huws SA, Cameron SJ, Lewis PD, Lewis KE . Lung cancer: A new frontier for microbiome research and clinical translation. Ecancermedicalscience, 2018,12:866.
doi: 10.3332/ecancer.2018.866 pmid: 30263057 |
| [32] | Dong H, Huang D, Yuan M, Cai S . The characterization of lung microbiome in sputum of lung cancer patients with different clinicopathology. Am J Cancer Re, 2019,199:A5553. |
| [33] |
Yu GQ, Gail MH, Consonni D, Carugno M, Humphrys M, Pesatori AC, Caporaso NE, Goedert JJ, Ravel J, Landi MT . Characterizing human lung tissue microbiota and its relationship to epidemiological and clinical features. Genome Biol, 2016,17(1):163.
doi: 10.1186/s13059-016-1021-1 pmid: 27468850 |
| [34] |
Lee SH, Sung JY, Yong D, Chun J, Kim SY, Song JH, Chung KS, Kim EY, Jung JY, Kang YA, Kim YS, Kim SK, Chang J, Park MS . Characterization of microbiome in bronchoalveolar lavage fluid of patients with lung cancer comparing with benign mass like lesions. Lung Cancer, 2016,102:89-95.
doi: 10.1016/j.lungcan.2016.10.016 pmid: 27987594 |
| [35] |
Liu HX, Tao LL, Zhang J, Zhu YG, Zheng Y, Liu D, Zhou M, Ke H, Shi MM, Qu JM . Difference of lower airway microbiome in bilateral protected specimen brush between lung cancer patients with unilateral lobar masses and control subjects. Int J Cancer, 2018,142(4):769-778.
doi: 10.1002/ijc.31098 pmid: 29023689 |
| [36] |
Yan XM, Yang MX, Liu J, Gao RC, Hu JH, Li J, Zhang LJ, Shi YJ, Guo HR, Cheng JL, Razi M, Pang S, Yu XW, Hu S . Discovery and validation of potential bacterial biomarkers for lung cancer. Am J Cancer Res, 2015,5(10):3111-3122.
pmid: 26693063 |
| [37] |
Gallo RL . S. epidermidis influence on host immunity: More than skin deep. Cell Host Microbe, 2015,17(2):143-144.
doi: 10.1016/j.chom.2015.01.012 pmid: 25674978 |
| [38] | Wang L, Hao K, Yang T, Wang C . Role of the lung microbiome in the pathogenesis of chronic obstructive pulmonary disease. Chin Med J (Engl), 2017,130(17):2107-2111. |
| [39] |
Mayhew D, Devos N, Lambert C, Brown JR, Clarke SC, Kim VL, Magid-Slav M, Miller BE, Ostridge KK, Patel R, Sathe G, Simola DF, Staples KJ, Sung R, Tal-Singer R, Tuck AC, Van Horn S, Weynants V, Williams NP, Devaster JM, Wilkinson TMA . Longitudinal profiling of the lung microbiome in the AERIS study demonstrates repeatability of bacterial and eosinophilic COPD exacerbations. Thorax, 2018,73(5):422-430.
doi: 10.1136/thoraxjnl-2017-210408 pmid: 29386298 |
| [40] |
Wang Z, Singh R, Miller BE, Tal-Singer R, Van Horn S, Tomsho L, MacKay A, Allinson JP, Webb AJ, Brookes AJ, George LM, Barker B, Kolsum U, Donnelly LE, Belchamber K, Barnes PJ, Singh D, Brightling CE, Donaldson GC, Wedzicha JA, Brown JR, COPDMAP . Sputum microbiome temporal variability and dysbiosis in chronic obstructive pulmonary disease exacerbations: An analysis of the COPDMAP study. Thorax, 2018,73(4):331-338.
doi: 10.1136/thoraxjnl-2017-210741 pmid: 29269441 |
| [41] |
Arora S, Ahmad S, Irshad R, Goyal Y, Rafat S, Siddiqui N, Dev K, Husain M, Ali S, Mohan A, Syed MA . TLRs in pulmonary diseases. Life Sci, 2019,233:116671.
doi: 10.1016/j.lfs.2019.116671 pmid: 31336122 |
| [42] |
Zhou HT, Coveney AP, Wu M, Huang J, Blankson S, Zhao H, O’Leary DP, Bai ZJ, Li YP, Redmond HP, Wang JH, Wang J. Activation of both TLR and NOD signaling confers host innate immunity-mediated protection against microbial infection. Front Immunol, 2019,9:3082.
doi: 10.3389/fimmu.2018.03082 pmid: 30692992 |
| [43] |
Huffnagle GB, Dickson RP, Lukacs NW . The respiratory tract microbiome and lung inflammation: a two-way street. Mucosal Immunol, 2017,10(2):299-306.
doi: 10.1038/mi.2016.108 pmid: 27966551 |
| [44] |
He BK, Liu YY, Hoang TK, Tian XJ, Taylor CM, Luo M, Tran DQ, Tatevian N, Rhoads JM . Antibiotic-modulated microbiome suppresses lethal inflammation and prolongs lifespan in Treg-deficient mice. Microbiome, 2019,7(1):145.
doi: 10.1186/s40168-019-0751-1 pmid: 31699146 |
| [45] |
Mammen MJ, Sethi S . COPD and the microbiome. Respirology, 2016,21(4):590-599.
doi: 10.1111/resp.12732 pmid: 26852737 |
| [46] |
Voss M, Wonnenberg B, Honecker A, Kamyschnikow A, Herr C, Bischoff M, Tschernig T, Bals R, Beisswenger C . Cigarette smoke-promoted acquisition of bacterial pathogens in the upper respiratory tract leads to enhanced inflammation in mice. Respir Res, 2015,16(1):41.
doi: 10.1186/s12931-015-0204-8 |
| [47] |
Yadava K, Pattaroni C, Sichelstiel AK, Trompette A, Gollwitzer ES, Salami O, Von Garnier C, Nicod LP, Marsland BJ . Microbiota promotes chronic pulmonary inflammation by enhancing IL-17A and autoantibodies. Am J Respir Crit Care Med, 2016,193(9):975-987.
doi: 10.1164/rccm.201504-0779OC pmid: 26630356 |
| [48] |
Wang Z, Bafadhel M, Haldar K, Spivak A, Mayhew D, Miller BE, Tal-Singer R, Johnston SL, Ramsheh MY, Barer MR, Brightling CE, Brown JR . Lung microbiome dynamics in COPD exacerbations. Eur Respir J, 2016,47(4):1082-1092.
doi: 10.1183/13993003.01406-2015 pmid: 26917613 |
| [49] |
Bautista MV, Chen YJ, Ivanova VS, Rahimi MK, Watson AM, Rose MC . IL-8 Regulates Mucin Gene Expression at the Posttranscriptional Level in Lung Epithelial Cells. J Immunol, 2009,183(3):2159-2166.
doi: 10.4049/jimmunol.0803022 pmid: 19596978 |
| [50] |
Larsen JM . The immune response to Prevotella bacteria in chronic inflammatory disease. Immunology, 2017,151(4):363-374.
doi: 10.1111/imm.12760 pmid: 28542929 |
| [51] |
Negroni A, Pierdomenico M, Cucchiara S, Stronati L . NOD2 and inflammation: current insights. J Inflamm Res, 2018,11:49-60.
doi: 10.2147/JIR.S137606 pmid: 29483781 |
| [52] |
Couturier-Maillard A, Secher T, Rehman A, Normand S, De Arcangelis A, Haesler R, Huot L, Grandjean T, Bressenot A, Delanoye-Crespin A, Gaillot O, Schreiber S, Lemoine Y, Ryffel B, Hot D, Nùñez G, Chen G, Rosenstiel P, Chamaillard M . NOD2-mediated dysbiosis predisposes mice to transmissible colitis and colorectal cancer. J Clin Invest, 2013,123(2):700-711.
doi: 10.1172/JCI62236 |
| [53] |
Moghaddam SJ, Li HG, Cho SN, Dishop MK, Wistuba II, Ji L, Kurie JM, Dickey BF, DeMayo FJ. Promotion of lung carcinogenesis by chronic obstructive pulmonary disease-like airway inflammation in a K-ras-induced mouse model. Am J Respir Cell Mol Biol, 2009,40(4):443-453.
doi: 10.1165/rcmb.2008-0198OC pmid: 18927348 |
| [54] |
Jin CC, Lagoudas GK, Zhao C, Bullman S, Bhutkar A, Hu B, Ameh S, Sandel D, Liang XS, Mazzilli S, Whary MT, Meyerson M, Germain R, Blainey PC, Fox JG, Jacks T. Commensal microbiota promote lung cancer development via γδ T cells. Cell, 2019, 176(5): 998- 1013. e16.
doi: 10.1016/j.cell.2018.12.040 pmid: 30712876 |
| [55] |
Jungnickel C, Schmidt LH, Bittigkoffer L, Wolf L, Wolf A, Ritzmann F, Kamyschnikow A, Herr C, Menger MD, Spieker T, Wiewrodt R, Bals R, Beisswenger C . IL-17C mediates the recruitment of tumor-associated neutrophils and lung tumor growth. Oncogene, 2017,36(29):4182-4190.
doi: 10.1038/onc.2017.28 pmid: 28346430 |
| [56] | Zhou WM, Guo QR, Wang H, Wu ZB, Zhang JY . Research advances in the transformation of chronic obstructive pulmonary disease to lung cancer. Acta Pharm Sin, 2020,55(7):1410-1418. |
| 周雯敏, 郭乔如, 王会, 吴增宝, 张建业 . 慢性阻塞性肺疾病转化为肺癌的研究进展. 药学学报, 2020,55(7):1410-1418. | |
| [57] | Francescone R, Hou V, Grivennikov SI . Microbiome, inflammation, and cancer. Cancer J, 2014,20(3):181-189. |
| [58] |
Samadi AK, Bilsland A, Georgakilas AG, Amedei A, Amin A, Bishayee A, Azmi AS, Lokeshwar BL, Grue B, Panis C, Boosani CS, Poudyal D, Stafforini DM, Bhakta D, Niccolai E, Guha G, Rupasinghe HPV, Fujii H, Honoki K, Mehta K, Aquilano K, Lowe L, Hofseth LJ, Ricciardiello L, Ciriolo MR, Singh N, Whelan RL, Chaturvedi R, Ashraf SS, Kumara HMCS, Nowsheen S, Mohammed SI, Keith WN, Helferich WG, Yang XJ . A multi-targeted approach to suppress tumor-promoting inflammation. Semin Cancer Biol, 2015,35(Suppl.):S151-S184.
doi: 10.1016/j.semcancer.2015.03.006 |
| [59] | Tang Mq, Yang JJ, Xu XX . Research progress on association between chronic inflammation of lung and lung cancer. Int J Respir, 2017,37(11):849-853. |
| 唐敏强, 杨俊俊, 徐兴祥 . 肺部慢性炎症与肺癌相关性的研究进展. 国际呼吸杂志, 2017,37(11):849-853. | |
| [60] |
Chang SH, Mirabolfathinejad SG, Katta H, Cumpian AM, Gong L, Caetano MS, Moghaddam SJ, Dong C . T helper 17 cells play a critical pathogenic role in lung cancer. Proc Natl Acad Sci USA, 2014,111(15):5664-5669.
doi: 10.1073/pnas.1319051111 pmid: 24706787 |
| [61] | Moghaddam SJ, Ochoa CE, Sethi S, Dickey BF . Nontypeable haemophilus influenzae in chronic obstructive pulmonary disease and lung cancer. Int J Chron Obstruct Pulmon Dis, 2011,6(1):113-123. |
| [62] |
Sriram KB, Cox AJ, Sivakumaran P, Singh M, Watts AM, West NP, Cripps AW . Non-typeable Haemophilus Influenzae detection in the lower airways of patients with lung cancer and chronic obstructive pulmonary disease. Multidiscip Respir Med, 2018,13(1):11.
doi: 10.1186/s40248-018-0123-x |
| [63] |
Berenson CS, Murphy TF, Wrona CT, Sethi S . Outer membrane protein p6 of nontypeable Haemophilus influenzae is a potent and selective inducer of human macrophage proinflammatory cytokines. Infect Immun, 2005,73(5):2728-2735.
doi: 10.1128/IAI.73.5.2728-2735.2005 pmid: 15845475 |
| [64] |
Barta P, Van Pelt C, Men T, Dickey BF, Lotan R, Moghaddam SJ . Enhancement of lung tumorigenesis in a Gprc5a Knockout mouse by chronic extrinsic airway inflammation. Mol Cancer, 2012,11:4.
doi: 10.1186/1476-4598-11-4 pmid: 22239913 |
| [65] |
Luo JL, Maeda S, Hsu LC, Yagita H, Karin M . Inhibition of NF-κB in cancer cells converts inflammation- induced tumor growth mediated by TNFα to TRAIL-mediated tumor regression. Cancer Cell, 2004,6(3):297-305.
doi: 10.1016/j.ccr.2004.08.012 |
| [66] |
Kovaleva OV, Romashin D, Zborovskaya IB, Davydov MM, Shogenov MS, Gratchev A . Human lung microbiome on the way to cancer. J Immunol Res, 2019,2019:1394191.
doi: 10.1155/2019/1394191 pmid: 31485458 |
| [67] |
Caetano MS, Zhang HY, Cumpian AM, Gong L, Unver N, Ostrin EJ, Daliri S, Chang SH, Ochoa CE, Hanash S, Behrens C, Wistuba II, Sternberg C, Kadara H, Ferreira CG, Watowich SS, Moghaddam SJ . IL6 blockade reprograms the lung tumor microenvironment to limit the development and progression of K-ras-mutant lung cancer. Cancer Res, 2016,76(11):3189-3199.
doi: 10.1158/0008-5472.CAN-15-2840 pmid: 27197187 |
| [68] |
Segal LN, Clemente JC, Tsay JCJ, Koralov SB, Keller BC, Wu BG, Li YH, Shen N, Ghedin E, Morris A, Diaz P, Huang L, Wikoff WR, Ubeda C, Artacho A, Rom WN, Sterman DH, Collman RG, Blaser MJ, Weiden MD . Enrichment of the lung microbiome with oral taxa is associated with lung inflammation of a Th17 phenotype. Nat Microbiol, 2016,1:16031.
doi: 10.1038/nmicrobiol.2016.31 pmid: 27572644 |
| [69] |
Huang YJ, Nariya S, Harris JM, Lynch SV, Choy DF, Arron JR, Boushey H . The airway microbiome in patients with severe asthma: Associations with disease features and severity. J Allergy Clin Immunol, 2015,136(4):874-884.
doi: 10.1016/j.jaci.2015.05.044 pmid: 26220531 |
| [70] | Vollenweider DJ, Frei A, Steurer-Stey CA, Garcia- Aymerich J, Puhan MA. Antibiotics for exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev, 2018, 10(10): CD010257. |
| [1] | Liumei Jian, Yingjie Xiao, Jianbing Yan. De novo domestication: a new way for crop design and breeding [J]. Hereditas(Beijing), 2023, 45(9): 741-753. |
| [2] | Qingyu Sun, Yang Zhou, Lijuan Du, Mengke Zhang, Jiale Wang, Yuanyuan Ren, Fang Liu. Analysis between macrophage-related genes with prognosis and tumor microenvironment in non-small cell lung cancer [J]. Hereditas(Beijing), 2023, 45(8): 684-699. |
| [3] | Jun Ma, Anping Fan, Wusheng Wang, Jinchuan Zhang, Xiaojun Jiang, Ruijun Ma, Sheqiang Jia, Fei Liu, Chuchao Lei, Yongzhen Huang. Analysis of genetic diversity and genetic structure of Qinchuan cattle conservation population using whole-genome resequencing [J]. Hereditas(Beijing), 2023, 45(7): 602-616. |
| [4] | Shuyu Mao, Changrui Zhao, Chang Liu. The nuclear receptor REV-ERBα integrates circadian clock and energy metabolism [J]. Hereditas(Beijing), 2023, 45(2): 99-114. |
| [5] | Hongyu Dai, Dong Ji, Cheng Tan, Jie Sun, Hao Yao. Research progress on the role and regulatory mechanism of pathogenic Th17 cells in neuroinflammation [J]. Hereditas(Beijing), 2022, 44(4): 289-299. |
| [6] | Jie Kou, Yan Li, Peng Wang, Hong Liu, Jiawen Liu, Juan Wang, Ye Wang, Liang Zhang, Fujun Shen. Optimization of microsatellite genotyping system used for genetic diversity evaluation of Ailuropoda melanoleuca [J]. Hereditas(Beijing), 2022, 44(3): 253-266. |
| [7] | Guoqing Qian. Advances in genome-wide association study of chronic obstructive pulmonary disease [J]. Hereditas(Beijing), 2020, 42(9): 832-846. |
| [8] | Zhiwei Xu, Yunlin Wei, Xiuling Ji. Progress on phage genomics of Pseudomonas spp. [J]. Hereditas(Beijing), 2020, 42(8): 752-759. |
| [9] | Yali Hu, Rui Dai, Yongxin Liu, Jingying Zhang, Bin Hu, Chengcai Chu, Huaibo Yuan, Yang Bai. Analysis of rice root bacterial microbiota of Nipponbare and IR24 [J]. Hereditas(Beijing), 2020, 42(5): 506-518. |
| [10] | Jianmin Zheng,Jiangtao Luo,Hongshen Wan,Shizhao Li,Manyu Yang,Jun Li,Ennian Yang,Yun Jiang,Yubin Liu,Xiangquan Wang,Zongjun Pu. Pedigree and development of wheat varieties in Sichuan Province [J]. Hereditas(Beijing), 2019, 41(7): 599-610. |
| [11] | Baojun Wu,Zhuo Wang,Yu Dong,Yuliang Deng,Qihui Shi. Identification and single-cell sequencing analysis of rare tumor cells in malignant pleural effusion of lung cancer patients [J]. Hereditas(Beijing), 2019, 41(2): 175-184. |
| [12] | Yue Shi,Zhengzheng Xu,Huan Lu,Weimin Ci. Correlation studies of distinct mutational signatures with common cancer pathological subtyping [J]. Hereditas(Beijing), 2018, 40(11): 1033-1038. |
| [13] | Siling Fu,Wanying Zhao,Wenjing Zhang,Hai Song,Hongbin Ji,Nan Tang. Hippo signaling pathway in lung development, regeneration, and diseases [J]. Hereditas(Beijing), 2017, 39(7): 597-606. |
| [14] | Xin Zhou,Weiyun Li,Hongyan Wang. The roles and mechanisms of MST1/2 in the innate immune response [J]. Hereditas(Beijing), 2017, 39(7): 642-649. |
| [15] | Wang Shiming, Song Xiao, Zhao Xueying, Chen Hongyan, Wang Jiucun, Wu Junjie, Gao Zhiqiang, Qian Ji, Bai Chunxue, Li Qiang, Han Baohui, Lu Daru. Association between polymorphisms of autophagy pathway and responses in non-small cell lung cancer patients treated with platinum-based chemotherapy [J]. Hereditas(Beijing), 2017, 39(3): 250-262. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||